Hot or Cold
Hot and cold treatments are among the most commonly used non-pharmacological methods for relief of muscle, tendon, ligament, and spinal pains.
Patients frequently ask us whether they should be applying a hot or cold compress to an area to help with their pain. Also, the frequency and duration with which they should be applied is a common cause for debate. Below we discuss the rationale for the use of hot and cold therapies and the potential effects that they may have.
What should I use – hot or cold?
The short answer is ‘either’. For most conditions, either hot or cold can be used. The reason for this, apart from in the most acute stages of an injury, is that hot or cold compresses are essentially being used to help with the sensation of pain.
Both hot and cold work using the pain gate mechanism – meaning that by applying hot or cold, the feeling of warmth (or cold) can, at least partly, override the sensation of pain so that your brain will detect the temperature rather than the pain itself.
Rubbing an area that is painful works in the same way. The sensation of the rubbing partly blocks out the feeling of the pain. TENS machines also work in this way. The stimulation of the skin distracts the brain by sending messages up the spinal cord which the brain will then focus on instead of the sensation of pain.
Think of this like turning up your TV to mask the sound of noisy neighbours. Below shows the more scientific explanation of how this works known as the ‘pain gate throry’.
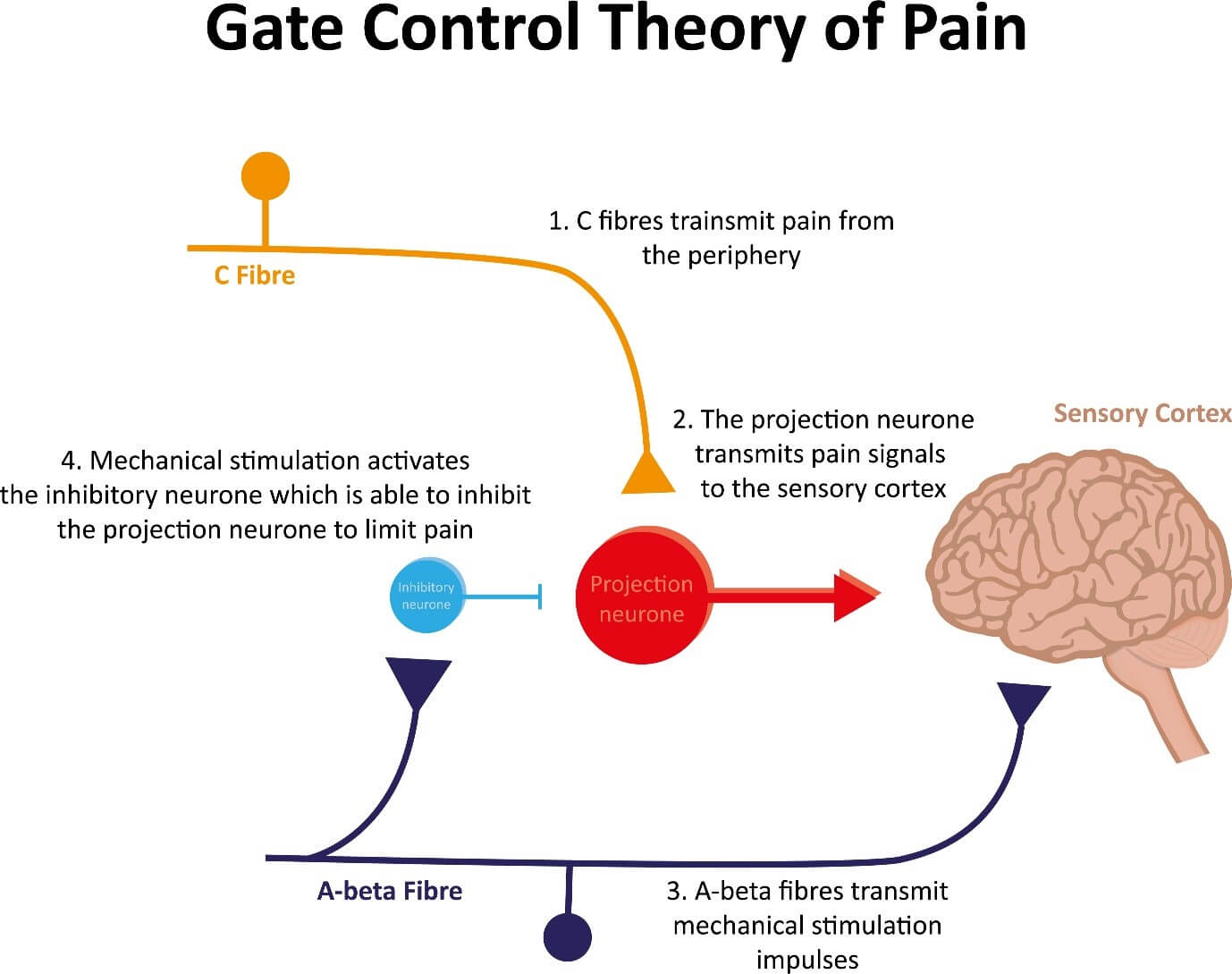
(Melzack and Wall’s pain gate mechanism)
What does cold therapy (cryotherapy) do?
- Relieves pain via the pain gate mechanism (see above)
- Reduces skin temperature
- Reduces blood flow
- Reduces inflammatory mediators
- Limits further tissue damage in acute trauma
- Causes local anesthesia (neurapraxia)
- Reduces local muscle spasm
Note that cold therapy can cause local ice burns and allergic reactions to the skin so should always be applied carefully, protecting the skin from direct contact with the ice. If in doubt, seek advice. Avoid where there is poor circulation, e.g. cardiovascular conditions, diabetes or reduced sensation.
What does heat therapy (thermotherapy) do?
- Relieves pain via the pain gate mechanism (see above)
- Increases local blood flow in tissues
- Reduces local muscle spasm
- May reduce DOMS (delayed onset muscle soreness)
Note that heat therapy can cause burns if the skin is not sufficiently protected. Avoid where there is poor circulation, e.g. cardiovascular conditions, diabetes or reduced sensation.

So which is better, hot or cold?
For most conditions, it is really a question of preference. In other words, there is no physiological advantage to using either hot or cold, with the possible exception of a very new/acute injury or post-surgical swelling (see below). However, the benefit of cold in these specific situations is debatable, likely to be very small, and it is thought that the compression and elevation account for most of the difference, rather than the cold itself.
Most studies that have compared the use of hot versus cold therapy have shown no significant difference in outcome between the two groups. This has been tested for a variety of musculoskeletal conditions including muscle soreness, and acute neck and low back pains.
But surely ice is better for acute injuries?
Whilst this is a commonly held belief there is actually surprisingly little good quality evidence to support it.
There is some weak evidence that cold therapy may give minor benefit for acute soft tissue injuries however most studies considered ice within the context of PRICE (protection, rest, ice, compression, and elevation) and so the exact influence of cold therapy as a standalone treatment is not clear.
The Association of Chartered Physiotherapists in Sports Medicine updated their guidelines in 2010 based upon systematic reviews of the evidence for acute soft tissue injury management.
The evidence concluded that cold therapy can achieve a (local numbing pain relief) analgesic effect after treatment lasting 5-15 minutes. It was however thought unlikely that it produced a significant reduction in swelling. There was some evidence that swelling following surgery was reduced using cryotherapy but this also often involved movement and elevation in the studies.
The reason why cold therapy has little impact ion swelling can be explained by the fact that the required reduction in temperature (5-15 degrees) lower local cell metabolism to reduce swelling and tissue damage would be extremely difficult to achieve. In studies, temperature tests as little as 1cm below the surface of the skin, show only minor changes in temperature following application of ice to the skin surface for prolonged periods.
Indeed, the lowest reported superficial muscle temperature (1cm below the skin), even after icing for a prolonged period, was found to be 21°c and this was in a population of athletes who are likely to have less body fat (subadipose tissue) than the general population and therefore would have been expected to have had a greater reduction in temperature monitored within the muscle.
Studies have looked at intra-articular (the temperature within the joint) following orthopedic surgery where ice is applied to the area. Once again, the detected changes were modest being just 3-4°. Our body has an extremely efficient thermo-protective layer designed to maintain our body’s temperature even in the extreme cold.
There is evidence of reduced blood flow in local tissues from cryotherapy (Nadler et al., 2004) which may potentially reduce metabolism sufficiently to limit some secondary tissue damage although the significance of this in terms of overall favourable outcomes from injuries has not been fully proven.
Conclusion
At Complete Physio we see thousands of patients every year and one of the most commonly asked questions is whether to apply either a hot or a cold compress to an area to relieve their symptoms and reduce swelling.
Whilst heat packs and cold packs are considered part of the standard of care for many injuries, much of the advice available on-line is based upon poor or empirical evidence.
There is evidence that both hot and cold therapy may give some pain relief through the pain gate mechanism and ice may provide temporary local analgesic effects.
However, there is minimal evidence for the reduction of swelling or any other significant physiological benefits. Both hot and cold may reduce muscle soreness and possibly help relieve muscle spasms.
So, aside of very acute injuries and post-surgical swelling which may respond slightly more favourably to cryotherapy, it is really a question of preference.
Indeed, many patients find that alternating between hot and cold (known as contrast therapy) can be very effective. This prevents the brain from becoming used to one mode of distraction and many patients find this to be more effective than just using hot or cold.
Guidelines based on good quality studies, suggest that hot or cold produces an effect of local pain relief after around 15 mins of application. This can be repeated 3-4 times each day at regular intervals. The skin should always be well protected (e.g. by a towel) to prevent damage from direct exposure or contact with hot or cold. Both hot or cold should be avoided where there is poor circulation e.g. for people with cardiovascular conditions or diabetes or reduced sensation due to increased risks of burns or local tissue damage.
If you would like some further information, please do not hesitate to contact us on info@complete-physio.co.uk or to make an appointment with one of our experienced practitioners to help you manage an injury, please call 0207-482-3875.
References
van den Bekerom, M.P., Struijs, P.A., Blankevoort, L., Welling, L., Van Dijk, C.N. and Kerkhoffs, G.M., 2012. What is the evidence for rest, ice, compression, and elevation therapy in the treatment of ankle sprains in adults?. Journal of athletic training, 47(4), pp.435-443.
Bleakley, C., McDonough, S. and MacAuley, D., 2004. The use of ice in the treatment of acute soft-tissue injury: a systematic review of randomized controlled trials. The American journal of sports medicine, 32(1), pp.251-261.
Bleakley, C.M., O’Connor, S.R., Tully, M.A., Rocke, L.G., MacAuley, D.C., Bradbury, I., Keegan, S. and McDonough, S.M., 2010. Effect of accelerated rehabilitation on function after ankle sprain: randomised controlled trial. Bmj, 340.
Bleakley, C.M., Glasgow, P. and MacAuley, D.C., 2012. PRICE needs updating, should we call the POLICE?.
Ernst, E. and Fialka, V., 1994. Ice freezes pain? A review of the clinical effectiveness of analgesic cold therapy. Journal of pain and symptom management, 9(1), pp.56-59.
Malanga, G.A., Yan, N. and Stark, J., 2015. Mechanisms and efficacy of heat and cold therapies for musculoskeletal injury. Postgraduate Medicine, 127(1), pp.57-65.
Nadler, S.F., Weingand, K. and Kruse, R.J., 2004. The physiologic basis and clinical applications of cryotherapy and thermotherapy for the pain practitioner. Pain physician, 7(3), pp.395-400.
Petrofsky, J., Berk, L., Bains, G., Khowailed, I.A., Lee, H. and Laymon, M., 2017. The efficacy of sustained heat treatment on delayed-onset muscle soreness. Clinical Journal of Sport Medicine, 27(4), pp.329-337.
Don’t let pain hold you back, book now!







