What is osteoarthritis of the hip?
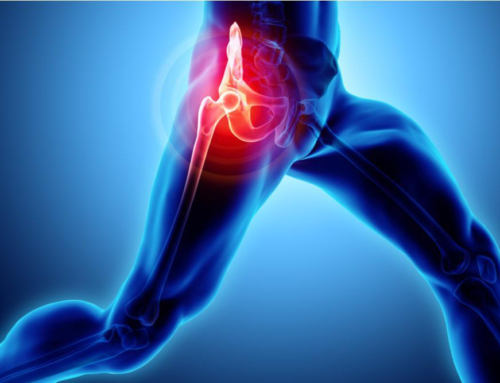
Osteoarthritis is a very common condition that many people develop as they get older. It can occur in any joint in the body, but most often develops in weight-bearing joints, such as the hips and knees. It is a condition that is caused by wear and tear on the articular cartilage in the joint.
The most widely reported symptoms of osteoarthritis of the hip are pain and stiffness; with pain often starting in the groin, and radiating down the leg or into the back. It can make it hard to complete everyday activities and tasks, like bending over to tie a shoe, rising from a chair, doing stairs, or taking a short walk.
Because osteoarthritis gradually gets worse over time, it’s important that you get an accurate diagnosis and begin treatment as soon as possible, in order to lessen its impact on your life. Although there is no cure for osteoarthritis, there are many treatment options available to you, to help you manage your pain and symptoms and stay active.
Anatomy of the hip joint
The hip joint is the largest, and one of the most important in the body. It consists of a ball (femoral head) at the top of the thigh bone (femur), which fits into a socket (acetabulum) in your pelvis; this is called a ball and socket joint.
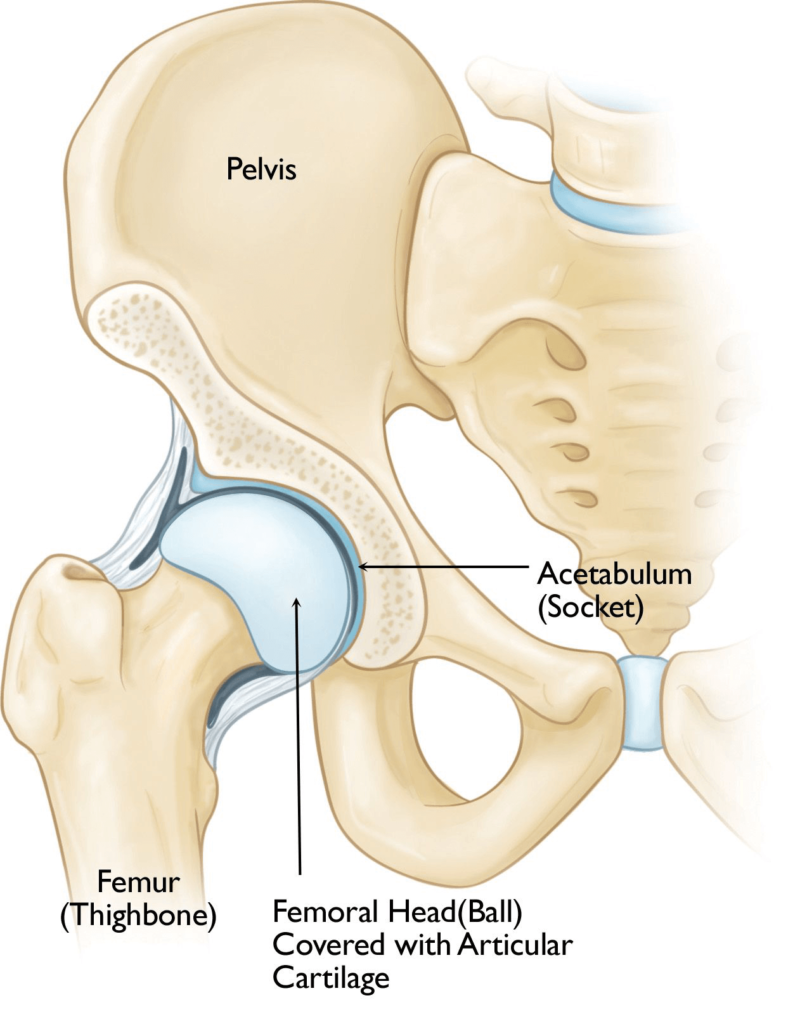
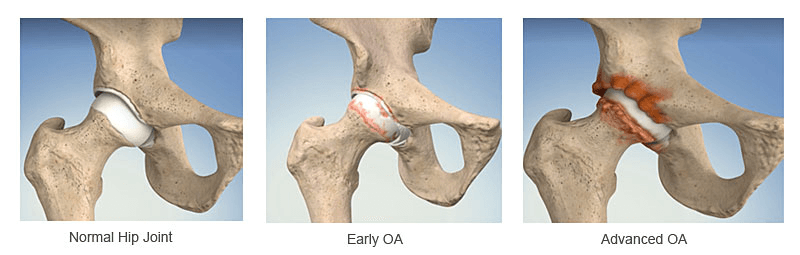
The bone surfaces of the hip joint are covered by a smooth, slippery surface called articular cartilage. This is tough tissue that cushions the ends of the bones and allows them to move easily, without friction. As well as providing smooth movement within the joint, it also functions as a “shock absorber.”
Osteoarthritis causes the cartilage in your hip to wear down and become thinner, which makes the surfaces rough and jagged. The thinner layer of cartilage and reduced shock absorbency, also means that the joint is more compressed, with greater forces going through it, causing microtrauma within the joint. As the disease process becomes more advanced over time, the body starts to make extra bone as a way of trying to protect the joint; these are called osteophytes. Unfortunately, this just adds to the problem causing more joint stiffness and inflammation. OA of the hip can be extremely debilitating and can significantly affect someone’s quality of life.
What causes Hip Osteoarthritis?
Osteoarthritis is a degenerative type of arthritis that occurs most often in people 50 years of age and older, though it can also occur in younger people, too.
The causes of osteoarthritis of the hip are not fully known.
Risk Factors
- Increasing age
- Family history of osteoarthritis
- Previous hip joint injury
- Lower limb muscle weakness
- Obesity
- Poor lower limb biomechanics
- Genetics or poorly formed joints
- Occupation/activities involving heavy lifting or high impact movements on the hip
What are the Symptoms of Hip Osteoarthritis?
A combination of pain and stiffness are the principal symptoms of hip arthritis. Everyday tasks such as stairs, bending, kneeling, putting on your socks and shoes, and even walking, gradually become more difficult.
Pain from an arthritic hip is classically located in the groin and buttock, although it often also radiates down the thigh, or even below the knee. The pain is usually described as a deep, dull, toothache pain that can be difficult to localise. Activity aggravates the pain while rest relieves it; however as the problem gets worse, the pain can linger, even at rest. Stiffness can be worse in the morning or after a period of prolonged sitting, which eases slowly once up and moving. Night pain is particularly distressing to patients and an indication of the severity of the condition.
Symptoms usually develop slowly and worsen over time; following a pattern of episodic ‘flare ups’ which last a few weeks, but then settle down with rest and treatment. These ‘flare ups’ gradually become more frequent and debilitating, and take longer to settle.
Most common symptoms include:
- Pain in the groin, thigh, buttocks or down your leg to the knee.
- Grinding noise (“Crepitus”) and “locking” or “sticking” when you move your hip.
- Hip stiffness, particularly morning stiffness.
- Aggravated by activities such as walking, putting on your socks and crossing your legs.
- Night pain, as the condition progresses.
If you are suffering from any of the above symptoms, or suspect that you have Hip Osteoarthritis then please get in touch to book an initial appointment. You can either call us on 0207 482 3875 or send us an email at info@complete-physio.co.uk and we will get back to you asap.
How is Osteoarthritis of the Hip Diagnosed?
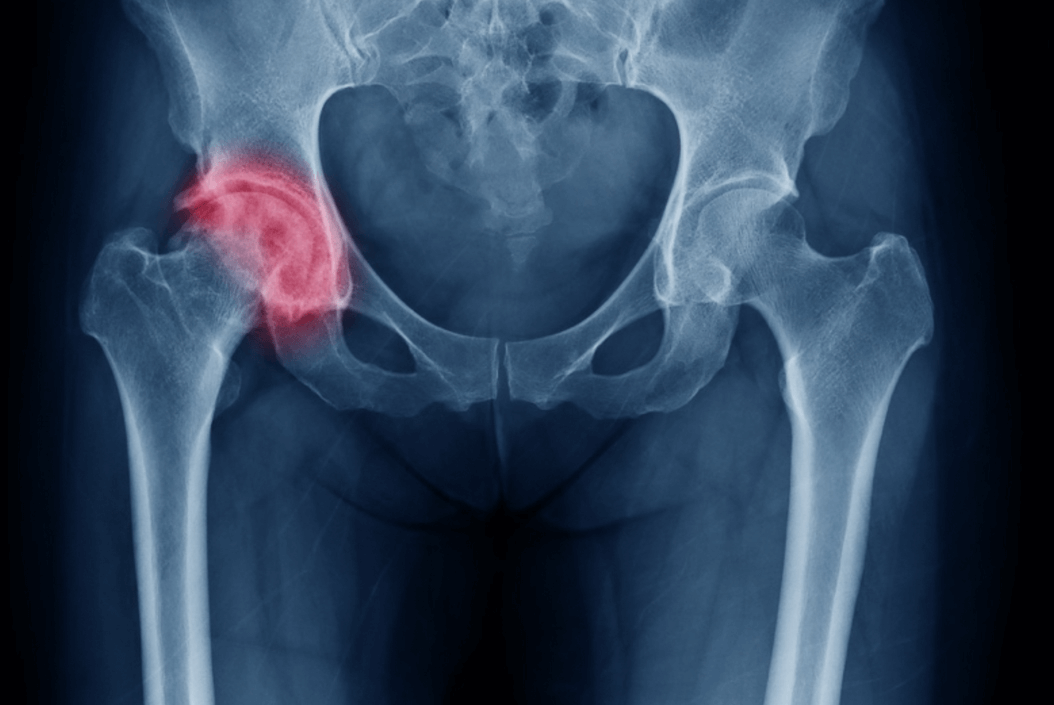
X-ray
Hip osteoarthritis is formally diagnosed on an X-ray. X-rays show bone very clearly, and will assess the serenity of the joint changes, and the stage of the arthritis.
X-rays of an arthritic hip may show a narrowing of the joint space, changes in the bone, and the formation of bone spurs (osteophytes.)
Your GP will be able to refer you quickly and easily for an X-xray on the NHS, or if you have medical insurance you may be able to get this done privately.
You may also need to have some blood tests to rule out any other systemic reasons for your pain such as rheumatoid arthritis.
It is important to note that most people over the age of 50 will very likely have visible osteoarthritic bone changes on X-ray, however they may not report any symptoms. Some patients may have significant OA changes visible on X-ray, but only minimal pain, whereas on the other hand, there are people whose images show extremely mild joint changes, but who describe substantial discomfort and symptoms, which greatly affects their quality of life.
Diagnostic Ultrasound
At Complete we are able to offer a unique service, as many physiotherapists are also highly experienced sonographers, who are able to carry out a diagnostic ultrasound of your hip and the surrounding soft tissues, at your initial appointment. This is a very useful investigation for hip pain as it assesses the surrounding soft tissues, as well as the joint. Research has shown that ultrasound imaging combined with a clinical assessment is highly sensitive at picking up early joint changes such as synovitis (joint inflammation) which can be responsible for the pain associated with osteoarthritis.
If you would like to have a diagnostic ultrasound, you will need to make sure you are booked in to see one of our Clinical Specialists; please mention this when you speak to our booking team.
MRI
MRI is generally not needed, except in circumstances when soft tissue problems, labral tears or loose bodies in the joint are suspected. If you do require an MRI your physiotherapist will be able to refer you to a recommended centre.
Clinical Assessment
At Complete our expert Physiotherapists will also carry out a full clinical assessment to ensure that your treatment is based on the whole clinical picture, not just on an X-ray image.

Your assessment will start with a consultation to gather information on your symptoms, aggravating and easing factors, your past medical history, and your normal exercise level. Your Physiotherapist will also spend time discussing what your rehab goals are.
Your physio will then complete a series of clinical tests to help confirm a diagnosis and collect some baseline, clinical measurements. Depending on the severity of your symptoms, these may include:
- Measuring the range of movement of your hip.
- Looking for joint swelling, warmth, or redness
- Feeling for crepitus (a grating sensation inside the joint) with movement.
- Assessing strength of the muscles around your lower leg and hips.
- Assessing muscle length and flexibility.
- Watching you move your hip, and how you perform activities such as walking, squatting, jumping, running.
- Gently, but skilfully, feeling around your hip joint to find exactly where it is most painful.
- Functional tests – If your pain is present during a specific activity or task, you may be asked to perform these, so the physiotherapist can assess exactly what is aggravating your pain.
- Assessing signs of injury to the muscles, tendons, and ligaments surrounding the hip.
How Do We Treat Osteoarthritis of the Hip?
It is not possible to reverse the bone and joint changes that occur with hip osteoarthritis, however there are a number of treatment options available to help reduce your pain and symptoms, and allow you to live a full and active life.
Research suggests that physiotherapy plays a key role in the management of osteoarthritis; by maintaining good flexibility and strength around the joint, it can help to slow disease progression.
Your muscles act as shock absorbers around the hip, therefore if you have strong hip and gluteal muscles, you will help reduce the forces going through the hip joint.
Hip osteoarthritis can respond well to physiotherapy and you should start to feel some benefit after a few sessions.

The main treatment goals of physiotherapy for your hip arthritis are:
- Reduce your hip pain and inflammation.
- Normalise your hip joint range of motion.
- Strengthen your lower limb muscles
- Normalise your muscle lengths.
- Improve your proprioception, agility and balance.
- Improve your functional movements and activity level, e.g. walking, squatting, climbing stairs.
Physiotherapy Treatment for Hip Arthritis
Your highly experienced physiotherapist will take you through a specific, tailored, rehabilitation programme, which may include:
- Relative Rest – Advice on rest and activity modification, and pacing yourself, to allow the pain and inflammation in your hip to settle.
- Patient Education – You will be given a clear explanation of your diagnosis and the causes of your symptoms; it’s important to understand your condition and to take an active role in your rehabilitation.
- Pain and Swelling Management – Ice can be applied to the affected area to help with pain and swelling. Painkillers and anti-inflammatory medication are often useful in the early stages of management (any medication needs to be approved by a pharmacist or doctor).
- Manual (hands on) Therapy – Your physiotherapist may use manual therapy such as joint mobilisations, stretches, massage or soft tissue release techniques to the surrounding muscles. This will help improve joint movement and reduce muscle stiffness or soreness.
- Range of Movement Exercise – Your physiotherapist may teach you some range of movement and stretching exercises, to help decrease joint stiffness and restore normal movement of your hip.
- Hip Strengthening Exercises – Your physiotherapist will design a safe resistance program to ensure all your lower limb muscle groups are strong.
- Proprioception and Balance Exercises – Any damage to your joints can affect your balance. These exercises will help your brain to reconnect with your hip, and give you a better sense of balance during movement and activities.
- Acupuncture – This can help with pain levels and muscle tightness around the joint.

- Biomechanical and movement re-education – Having a lower limb joint injury can cause altered movements, especially walking. Your physiotherapist may need to re- teach you how to correctly walk, squat, kneel, run, and/or any other specific activity. For some patients using walking supports like a walking stick, or crutches, can improve mobility and independence.
- Functional and Sports Specific Training – Once your pain, movement and strength improve, functional training working on more specific techniques, can help you safely resume more demanding activities and sports.
Throughout your sessions at Complete Physio, we will ensure that you feel involved in your rehab process and supported during your treatment.
You will very likely be given exercises to continue independently; this is a key component of your treatment programme and will require some commitment and consistency.
What if the pain is too severe to exercise?
Ultrasound Guided Injection Therapy for Hip Arthritis
If your pain and symptoms are not settling with physiotherapy and medication, an ultrasound guided steroid injection can provide very effective pain relief. Injections should always be followed up with a course of physiotherapy, as they are not a long term cure for your symptoms. However they can provide a window of opportunity to allow your symptoms to settle, for you to engage better with your rehabilitation.
Hyaluronic acid and PRP injections can provide an alternative to steroid injections and have been shown to be an effective option for osteoarthritis; research suggests that they can be effective in improving pain, joint range of movement, muscle strength and patients’ overall function.
Surgery for Hip Arthritis
Hip surgery is sometimes required as your hip joint arthritis deteriorates, and your symptoms become more debilitating and life limiting. The most common surgical procedure for an osteoarthritic hip is a total hip replacement, or sometimes your hip surgeon may recommend arthroscopic surgery or joint resurfacing.
Total hip replacement surgery is a highly successful surgical intervention and the prognosis following a total hip replacement is excellent. It offers reliable relief from pain plus considerable improvement in function, in patients suffering from osteoarthritis of the hip.
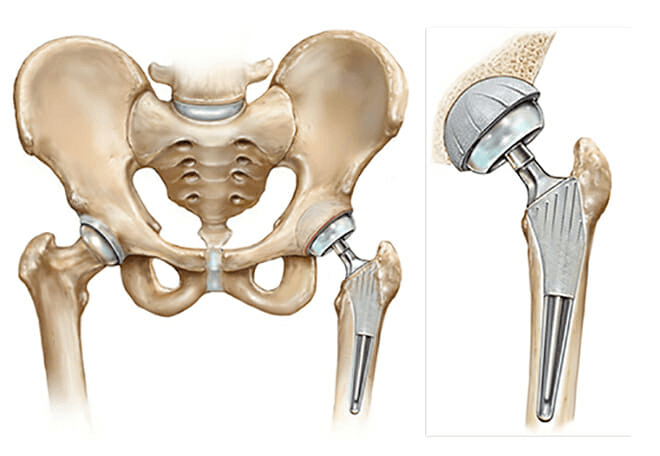
If an onward referral to an Orthopaedic Surgeon is required, we will ensure that you are provided with the best care possible; we work with some of the most experienced and highly regarded orthopaedic consultants in the country.
After surgery you will require a post-operative hip strengthening and rehabilitation program to prolong the life of your new hip and resume your most active lifestyle. You’ll be referred back to your physiotherapist at Complete for a course of post-operative rehabilitation to make sure you achieve the best possible outcome.
If you would like to book an appointment or speak to one of our expert physiotherapists about your hip, please call 020 7482 3875 or email info@complete-physio.co.uk.
Don’t let pain hold you back, book now!