What is Iliotibial Band (ITB) Syndrome?
ITB syndrome (also known as runner’s knee), is where a tendon called the iliotibial band gets irritated or swollen from compression against the lower end of your thigh (femur) bone where it attaches onto your knee. This compression causes friction resulting in inflammation and pain.
It’s a common overuse injury, often caused by activities where you bend your knee repeatedly, like running, cycling, hiking, and walking long distances.
What is the Iliotibial Band?

The iliotibial band is a thickened band of deep fascia that runs down the lateral (outside) surface of the leg, and it goes from the top of your pelvic bone down to below your knee.
Its primary function is to stabilise the hip and knee, and provide lateral support to the lower limb. This allows for a strong pillar-like structure on which we can stand (especially if standing on one leg) and helps to stabilise the pelvis during locomotion.
It also supports movements of the hip and knee through the action of the gluteus maximus and tensor fasciae latae muscles. These muscles actually insert into the ITB.
Anatomy of the Iliotibial band
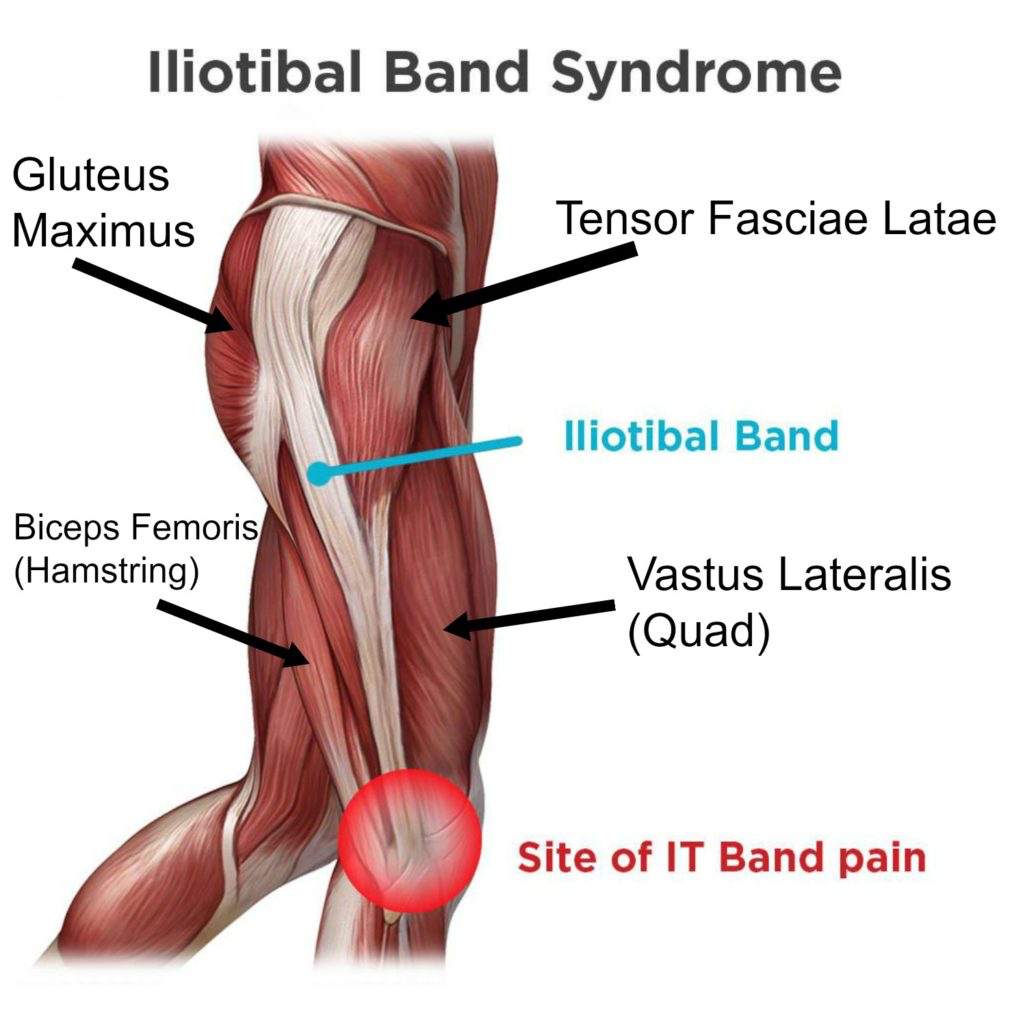
At the top of your thigh the Iliotibial Band is attached to your tensor fascia latae (TFL) muscle, and gluteus maximus and at the bottom it connects to your tibia (lower leg bone) and also your femoral condyle on the lower outside portion of the thigh bone (femur)..
What Causes Iliotibial Band Syndrome?
The problem is caused by compression and friction where the iliotibial band crosses over the outside of the knee. A fluid-filled sac called a bursa, helps the ITB glide smoothly over your knee as you bend and straighten your leg. Your ITB and the bursa can both start to become inflamed with repeated rubbing, which leads to the pain of Iliotibial Band Syndrome.
Common Causes of Iliotibial Band Syndrome:
- Poor biomechanics (running or cycling technique); mainly inwards rolling knees and hips
- Tightness in the hip / gluteal muscles
- Weak hip / gluteal muscles
- Weak inner quadricep (thigh) muscles
- Weak core muscles
- Poor foot arch control – flat feet
- Worn out or unsuitable trainers
- A sudden increase in mileage, or intensity of activity
- Excessive hill running training (mainly downhill)
- Endurance running or cycling (training for ½. and full marathons, ultra-marathons)
What are the Symptoms of Iliotibial Band Syndrome?
The main symptom of ITB syndrome is a sharp pain, burning or ache on the outside of your knee, which may spread down your leg, and occasionally up towards your hip. The outside of your knee may be tender to the touch and you may have some swelling. The pain is often worse when you run downhill, or if you run or cycle for longer than you normally would. You may find that the pain starts at a similar point in your run or cycle, and goes shortly after you stop.
Usually, you’ll only feel pain when you do the aggravating activity. But if the problem continues and gets worse, it can start to affect you even when you just go for a walk, bend, do stairs, or sit with your knees bent.
There are varying degrees of severity of ITB Syndrome.
The most common symptoms include:
- Sharp or burning pain just above the joint line, on the outer part of the knee.
- Pain that worsens with a continuance of running or other repetitive activities
- Swelling over the outside of the knee.
- Pain going down hill or walking downstairs.
- Gradual onset of symptoms which if they persist for greater than four weeks can cause significant sport or activity interference.
- Tenderness to touch on the bone on the outside of your knee.
If you have noticed any of these symptoms, or suspect that you have Iliotibial Band Syndrome, then please book in to see one of our expert physiotherapists.
You can call 0207 482 3875 or email info@complete-physio.co.uk. If you would like to speak to a specialist before booking, then please send us an email with your details and we will call you back.
How is Iliotibial Band Syndrome Diagnosed?
Making sure you get an accurate diagnosis of Iliotibial Band Syndrome is essential. It allows the clinician to select the most effective treatment plan for you. A diagnosis will be made by your physiotherapist by carrying out a comprehensive clinical assessment.
They will ask questions about your past health, progression of symptoms, your daily activities, and exercise routine, to build a picture of your likely diagnosis.
After your consultation, the specialist will complete a series of tests to help develop a diagnosis; this may include:
- Assessing the range of movement and strength of your knees and hips.
- Assess muscle length and flexibility of quadriceps, hamstrings and gluteal muscles.
- Watching you move your knee and how you perform activities such a s squatting, hopping, jumping, running.
- Checking other regions of the body as needed; such as feet and lower back. This will help to determine if other areas also require treatment to improve your condition.
- Gently, but skilfully, feeling around your knee joint and ITB to find exactly where it is most painful.
- Functional tests – You may be asked to perform specific activities that aggravate your pain, so the physiotherapist can assess exactly what is causing the problem.
The clinical assessment is normally sufficient to diagnose Iliotibial Band Syndrome. However, it is limited in providing any further information about the exact structures causing the inflammation, or whether there is swelling of the ITB itself and increased fluid in the busa or surrounding tissues.
We would certainly recommend that if your pain is not improving or you have been diagnosed with ITB friction syndrome but the pain is still present that you should book in with one of our expert physiotherapists.
Diagnostic Ultrasound for Iliotibial Band Syndrome?
A diagnostic ultrasound scan is the gold standard imaging test to discover if your pain is coming from iliotibial band syndrome. Diagnostic ultrasound is excellent at looking under the skin and identifying exactly which structures are involved in driving your pain. The advantage of ultrasound, over an MRI, is it can assess the structures dynamically and the scan can be carried out during the specific movement that causes your pain. Ultrasound can assess if your ITB is thickened and/or if you have any fluid between the ITB and the lateral femoral condyle (the bone on the outside of your knee). It can also help identify other conditions such as lateral meniscal tears, meniscal cysts and distal hamstring tendinopathy.
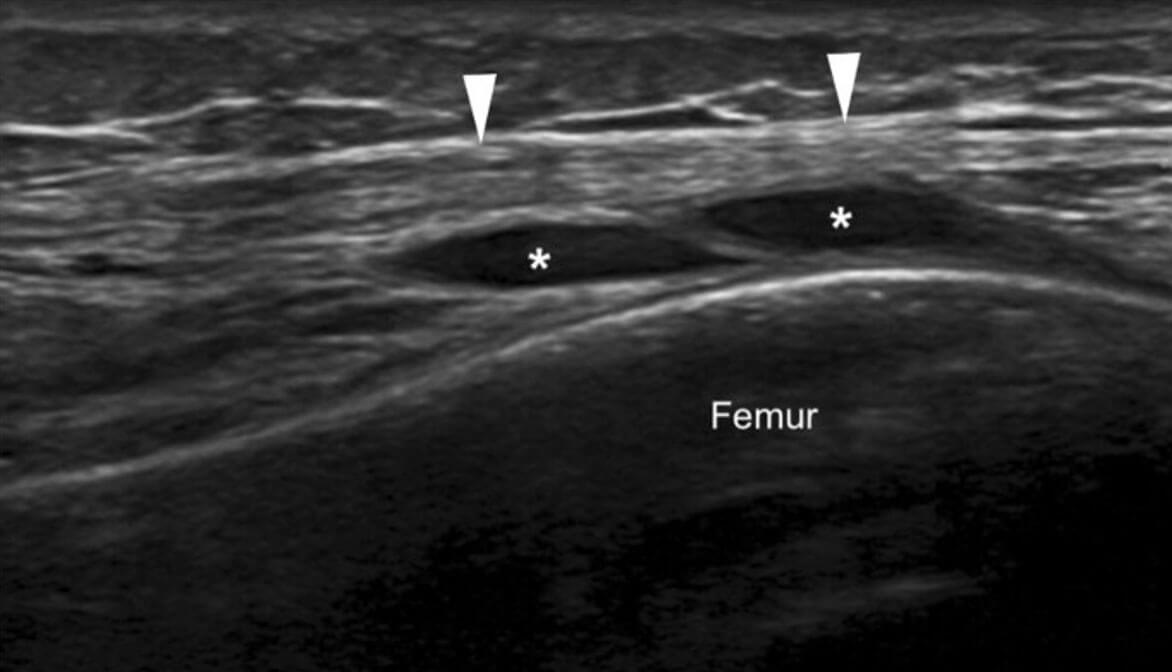
Longitudinal Ultrasound Image of the ITB with joint fluid underneath (*) tracking from the lateral (outside) of the knee joint
At Complete our Clinical Specialists carry out an ultrasound scan as part of their clinical assessment. We do not charge extra for an ultrasound scan, and you do not require a GP referral. If you would like to book an assessment with one of our clinical specialists, including an ultrasound scan, please ensure you inform our administration team at the time of booking.
To book an appointment to see one of our clinical specialists please call 0207 482 3875 or email info@complete-physio.co.uk.
MRI scan for Iliotibial Band Syndrome?
An MRI scan is not required for diagnosing ITB syndrome but can provide a useful image of the entire knee. This is particularly useful if we are unsure of your diagnosis. At Complete our physiotherapists can send you for an MRI if required.
An MRI scan is a static (not a dynamic scan, like diagnostic ultrasound) performed at rest with your knee straight. An MRI visualises the deeper structures in the joint better than ultrasound, such as the articular cartilage on the joint surfaces and it will pick up tears in the meniscus or cruciate ligaments. (please add links to these 2 pages when they have been uploaded)
X-Ray for Iliotibial Band Syndrome?
An X-ray will not help to diagnose a tendon problem as soft tissue does not show up on x-ray, however it will show any bony abnormalities or damage such as osteoarthritis or bone fractures.
What is the Treatment for Iliotibial Band Syndrome?
Physiotherapy for Iliotibial Band Syndrome.
At Complete Physio, every year we see a lot of ITB syndrome, especially during the training phase for an endurance running event, such as the London Marathon and also long distance cycling events such as Ride London. The majority of these cases resolve with a reduction in training load and physiotherapy alone.
Physiotherapy may involve:
- Modification of exercise and training schedule
- ITB friction syndrome focused strengthening exercises for both the hip and knee (and potentially ankle/foot)
- Stretching exercises for key lower limb muscles
- Hands on treatment to optimise soft tissue mechanics and balances
- ITB sports taping
- Running analysis
- Cycling assessment and bike fit
- Footwear assessment and advice regarding insoles (orthotics)
At Complete Physio we are highly experienced in treating ITB injuries, and your physiotherapist will take you through a specific, tailored rehabilitation programme based on your personal profile.
This will often include:
- Relative rest – Advice on rest and activity/training modification, allowing the pain and inflammation to settle and the ITB to heal appropriately.
- Patient education – It’s important to understand your condition and to be active in your recovery. You will be given a clear explanation of the diagnosis and any other underlying causes, and we will discuss what is needed in order to settle your symptoms and reach your treatment goals.
- Pain management – Taping the knee to offload and reduce the pressure on the ITB can also help to reduce your pain. Ice can be an excellent modality to help control pain, inflammation and swelling
- Range-of-movement exercise – Your physiotherapist may teach you active, self-stretching methods. They may also do some hands-on, passive stretching with you. Together, these can really help decrease muscle tightness or tension and restore normal motion of your joints.
- Manual therapy – Your physiotherapist may use manual therapy such as massage or soft tissue release techniques to the ITB and surrounding muscles. This will help improve movement and reduce muscle stiffness or soreness. ITB rollers are an excellent way to help release the ITB as part of your home exercise programme.
- Muscle strength – Muscle weaknesses or imbalances throughout the lower limb have been shown in the medical literature to contribute to ITB syndrome. Your physiotherapist will design a safe resistance program to ensure all your lower limb muscle groups are strong and working in synergy. They will also work on your core stability too as it is vital to have a strong centre in order to move your limbs effectively and efficiently.
- Biomechanical and movement re-education – This may involve assessing you doing a specific activity or movement such as running, squatting or jumping, and teaching you how to correct your technique, so that you are activating the correct muscles and moving more efficiently so that you do not aggravate your symptoms. At complete, we also offer specific running and cycling assessment clinics.
- Functional and sports specific training – Once your pain, strength, and range of movement improve, functional training can help you safely resume more demanding activities and get you back to playing the sport that you love.
- Podiatrist/Orthotics – your physiotherapist may advise you visiting a podiatrist to further assess your running and biomechanics. The podiatrist may advise customised insoles to control your foot mechanics to offload the painful area.
Throughout your treatment at Complete Physio, we will continue to monitor your progress by carrying out objective tests. We will also keep revisiting your personal goals, so that we ensure you feel supported and involved in your rehab process. We are dedicated to getting you back to full activity and function, and we have a highly skilled team of practitioners to ensure your goals are achieved.
If you have exhausted physiotherapy, or you quite simply are running out of time before the event, then ITB syndrome can respond very well to ultrasound-guided injection.
Ultrasound Guided Injections for Iliotibial Band Syndrome?
An ultrasound guided steroid injection should be considered if:
- Your pain is not improving despite activity modification.
- You have not improved with a course of physiotherapy.
- You have had a scan to confirm the exact diagnosis.
- You are running out of time and do not have time to engage in a course of physiotherapy prior to an event.
Steroid injections are strong anti-inflammatories, targeted directly to the area of concern. This will reduce the inflammation between the ITB and the femoral condyle and works particularly well if there is fluid and/or inflammation present, or thickening of the ITB (seen on ultrasound).

An ultrasound guided injection uses an ultrasound machine to directly target the damaged tissue. The target tissue is often a few millimetres in size and therefore guidance is essential to get the most effective outcome. Steroid injections can help to relieve the pain, but in addition your clinician will guide your return to running to ensure you do not overdo it. It is essential that a steroid injection is carried out in conjunction with physiotherapy.
The steroid injection itself is placed superficially and therefore does not enter into the knee joint, nor does it go directly around any tendons. injections can take 3-5 days to exert their effect and therefore, we normally advise anything between 3-7 days off running after the injection, depending on the scan findings and how severe your problem is.
If considering an injection to get you through a specific event, we recommend having the injection no less than 5-7 days beforehand, to maximise the effect and ensure you are ready to compete.
At Complete, while we want to get you to the starting line, we will never compromise the long-term health of your knee.
Surgery For ITB Syndrome
People with ITB syndrome rarely need surgery. This is only carried out as an absolute last resort and has unpredictable outcomes.
At Complete Physio we work with some of London’s most highly experienced and world renowned consultants. If you require an onward referral, we will ensure that you are provided with the best care possible, and will continue to support your recovery every step of the way. A physiotherapy guided rehabilitation programme will be needed following surgery to restore full movement and strength, and get you back to full activity.
If you would like to speak to one of our expert physiotherapists or to book an appointment please call 020 7482 3875 or email info@complete-physio.co.uk
Don’t let pain hold you back, book now!






