Osteoarthritis (OA) is inflammation of one or more of your joints. Pain, swelling (fluid on the knee), and stiffness are the primary symptoms of arthritis. Any joint in the body may be affected by the disease, but it is particularly common in the load bearing joints of the lower limb, especially the knee.
Knee OA is caused by wear and tear, and thinning of the cartilage in your knee joint which results in the bones of the joint compressing more closely against one another with less of the shock-absorbing benefits of cartilage. This extra load on the joint results in pain, swelling, stiffness, and sometimes, the formation of osteophytes (extra bone growth along the margins of the joint). The synovial membrane (thin layer of tissue) surrounding the joint can also become irritated and swollen (known as synovitis), causing swelling (also known as an ‘effusion’) and pain. These symptoms result in reduced walking mobility and general mobility, and over time can become very debilitating.
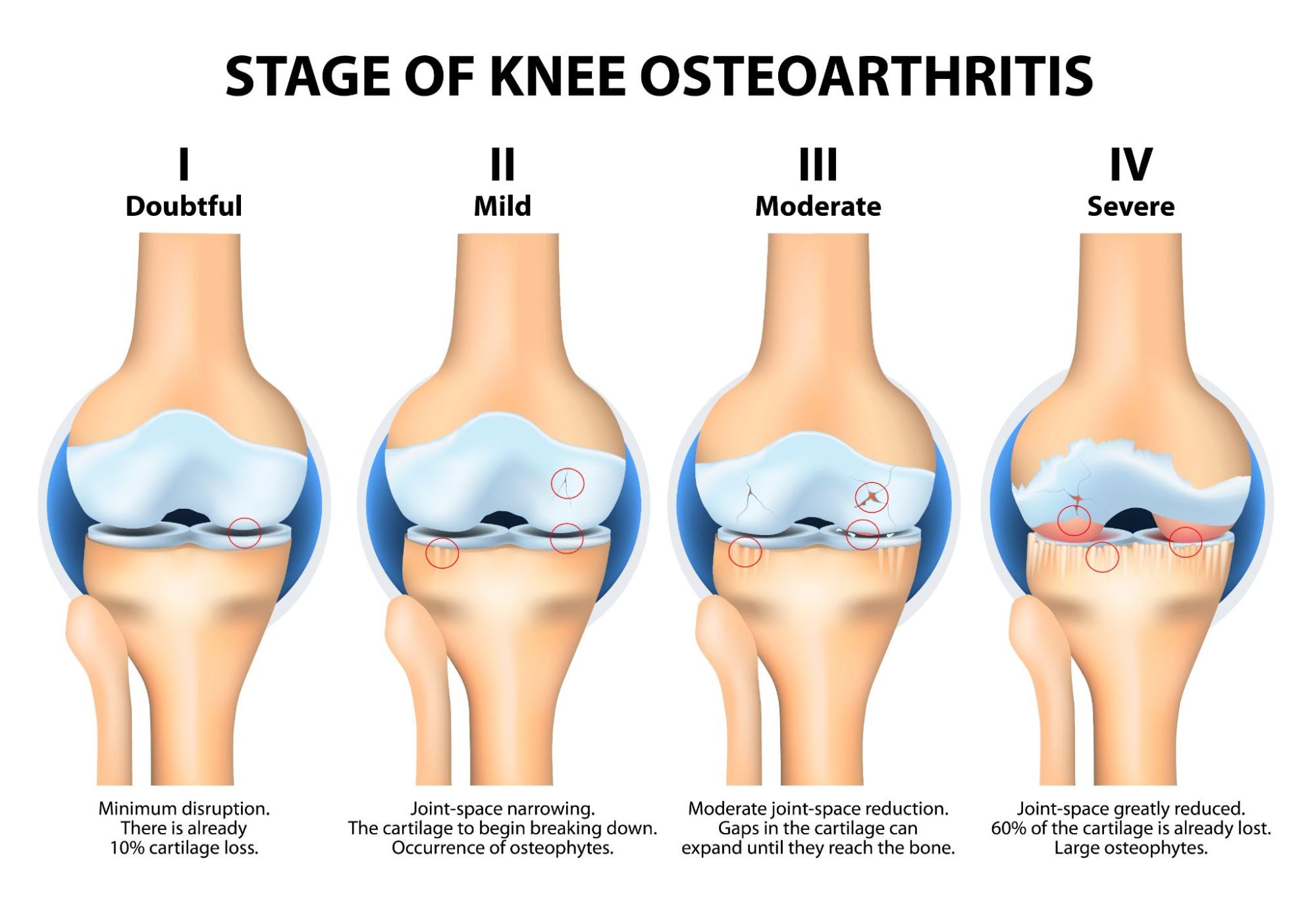
What are the stages of Knee osteoarthritis?
Stage 1 – Minor
In stage 1 OA, patients will develop very minor wear and tear. At this stage it is unlikely you will feel any pain or discomfort.
Stage 2 – Mild
In stage 2, diagnostic images or X-rays of knee joints will show more wear and tear and bone spur growth, and though the space between the bones appears normal, people will begin to experience joint pain.
Typically, the area around the knee joint will feel stiff and uncomfortable, particularly when sitting for an extended period, after rising in the morning, or after a workout.
Stage 3 – Moderate
Stage 3 is referred to as “moderate”, where there is obvious erosion of the cartilage surfaces between bones and the gap between the bones narrows. Bone spur growth will worsen and the joint surfaces will become rough.
With the progression of OA of the knee, there is obvious joint inflammation which causes more frequent pain. Stiffness will become worse and there may be popping or snapping sounds when walking.
Stage 4 – Severe
Stage 4 is considered to be severe. In stage 4 the joint space between the bones is considerably reduced, with the cartilage wearing through, leaving the joint feeling very stiff. The breakdown of cartilage leads to a chronic inflammatory response, with decreased synovial fluid causing friction, and greater discomfort moving the joint.
The advanced stage of the disease shows development of more bone spurs causing debilitating pain which makes even everyday tasks, including walking and descending stairs, a challenge. At this stage surgery is often indicated.
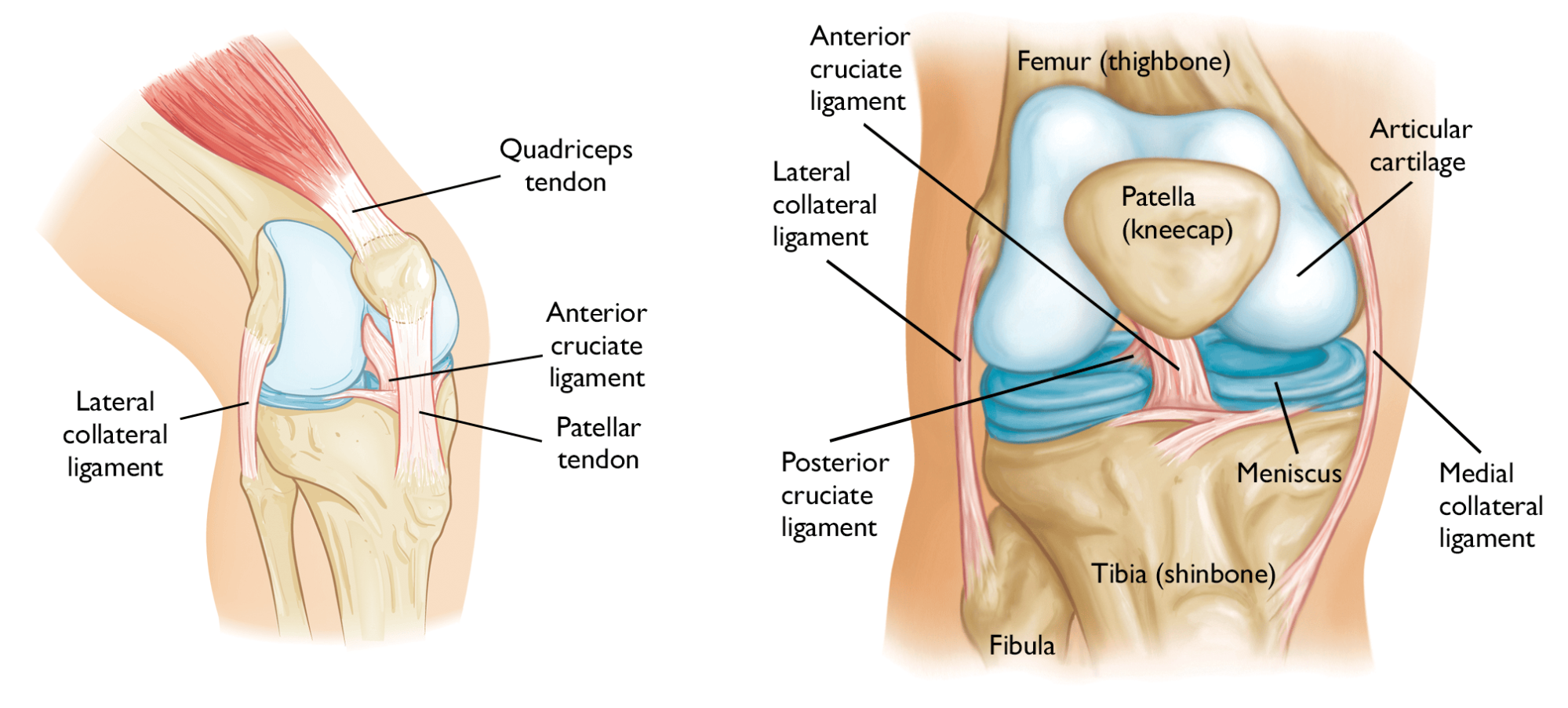
Anatomy of Knee osteoarthritis
The knee is one of the largest and strongest joints in your body. It is made up of the lower end of the femur (thighbone), the upper end of the tibia (shinbone), and the patella (kneecap). The ends of the three bones that form the knee joint are covered with articular cartilage, a smooth, slippery substance that protects and cushions the bones as you bend and straighten your knee, and put weight through it.
Two wedge-shaped pieces of cartilage called meniscus act as “shock absorbers” between your thigh bone and shinbone. They are tough and rubbery to help cushion the joint and keep it stable.
Ligaments connect the femur to the bones of the lower leg. The four main ligaments in the knee attach to the bones and act like strong ropes to hold them together.
The knee joint is surrounded by a thin lining called the synovial membrane. This membrane releases a fluid that lubricates the cartilage and reduces friction.
What are the causes of knee osteoarthritis?
Doctors don’t know exactly why some people develop osteoarthritis in their knees. But there are some things that can increase your risk.
Risk Factors for Knee osteoarthritis:
- Age: OA can occur at any time of life, but it is most common in older adults over 50.
- Sex: women are more likely to have knee OA than men. One large study suggested 19% of women suffer, compared to 13.5% of men.
- Obesity: your weight directly affects the amount of load the joints in your lower limb have to support during weight-bearing activities. Being overweight adds stress to your knees. Fat cells also make proteins that can cause inflammation in and around your joints.
- Injuries: any knee injury, even old ones, increases the likelihood of developing knee OA.
- Excessive stress: too much stress on your knee from your job, doing too much high impact exercise like high-mileage running or playing high impact sports could increase the risk of OA.
- Genetics: you can inherit a propensity to develop OA. People who have family members with OA are more likely to develop OA.
- Bone deformities: if you have altered bone or joint alignment, or any bony abnormalities, you are at higher risk.
- Some metabolic diseases: Diabetes and hemochromatosis, a condition in which your blood has too much iron, have been linked to OA.
What are the symptoms of knee osteoarthritis?
Osteoarthritis of the knee is a progressive, degenerative condition. This means it slowly gets worse over time. Initially you may notice only the occasional episode of knee pain and stiffness.
The pain can be felt all around your knee, or just in a certain place such as the front or sides. It might feel worse after moving your knee in a particular way, such as going up or down stairs.
The pain will vary according to whether both the inside (medial) and outside (lateral) of the knee joint are affected. If one compartment only is affected this is known as “unicompartmental” osteoarthritis. However, it is not uncommon that both compartments are affected in the same knee.
Sometimes, people have pain that wakes them up in the night. You’ll probably find that the pain varies and that you have good and bad days. Typically, pain and stiffness associated with osteoarthritis of the knee is worse first thing in the morning, or even after being sat still for a long time, and feels better once you get up and get moving. Some people describe increased symptoms with changes in the weather.
Over time these intermittent episodes of pain and stiffness may become more regular or start to affect activities of daily living including walking, exercise, or kneeling. You may also notice a change in shape of your knee (this is called bony deformation). This is a common symptom of well-established osteoarthritis of the knee.
What are the symptoms of Knee osteoarthritis?
- Pain: both movement and inactivity can cause pain. Regular, gentle movement may alleviate some of this pain.
- Stiffness: your knees may be stiff first thing in the morning or after sitting for a long time.
- Loss of motion: over time, you may lose the ability to bend and straighten your knee all the way.
- Creaking and grating (“crepitus”): you may hear crackling, clicking noises, or feel a grating sensation when you move your knee.
- Instability: your knee may “give out” or buckle, or feel like it could.
- Locking: the knee may lock or stick.
- Swelling: your knee may get puffy all around or on one side. It may also be red and warm to touch.
If you are experiencing any of these symptoms, or suspect that you have osteoarthritis of the knee, and would like to see one of our expert physiotherapists,please call 0207 482 3875 or email info@complete-physio.co.uk. If you would like to speak to a specialist before booking, then please send us an email with your details and we will call you back.
How is Knee Osteoarthritis Diagnosed?
Obtaining an accurate diagnosis is essential; it allows the clinician to select the most effective treatment plan for you. Your physiotherapist at Complete will firstly ask specific questions about the onset of your problem, past health, symptoms, and exercise regime. How the problem started and a description of symptoms often gives the clinician a clear hypothesis for your potential diagnosis.
After the history taking, your physio will complete a series of clinical tests to help confirm a diagnosis. Depending on the severity of your symptoms, these may include:
- Measuring the range of movement of your knee
- Looking for joint swelling, warmth, or redness
- Feeling for crepitus (a grating sensation inside the joint) with movement
- Assessing muscle strength, in particular the quadriceps at the front of your thigh and also the muscles around your lower leg and hips.
- Assessing muscle length and flexibility of quadriceps, hamstrings and calves.
- Watching you move your knee and how you perform activities such as walking, squatting, jumping, running.
- Gently, but skilfully, feeling around your knee joint to find exactly where it is most painful.
- Functional tests – If your pain is present during a specific activity or task, you may be asked to perform these, so the physiotherapist can assess exactly what is aggravating your pain.
- Assessing signs of injury to the muscles, tendons, and ligaments surrounding the knee.
X-Ray for Knee osteoarthritis
Whilst a clinical diagnosis of OA can usually be made following the assessment. A formal and definitive diagnosis of osteoarthritis of the knee requires an x-ray. An x-ray can assess the severity of degenerative change and can be requested quickly and easily by your GP. This is usually a very quick process as waiting times for x-rays are often short.
A reduction of joint space between the femur and tibia, which would indicate a loss of cartilage in the knee, can be seen on x-rays (see image below). In extreme cases, the two bones will be touching. Bone spurs (osteophytes) can also be seen on an x-ray.
It is important to remember that most people over 50 will have visible osteoarthritic changes in their knees on x-ray, even though many won’t have any symptoms. In fact, some people may have x-rays that show significant signs of knee OA but the individual will be pain-free, whilst other people may have images that only barely hint at the condition but describe substantial discomfort and symptoms.
Occasionally your GP may also request a series of blood tests. This is to rule out other causes of knee pain such as rheumatoid arthritis.
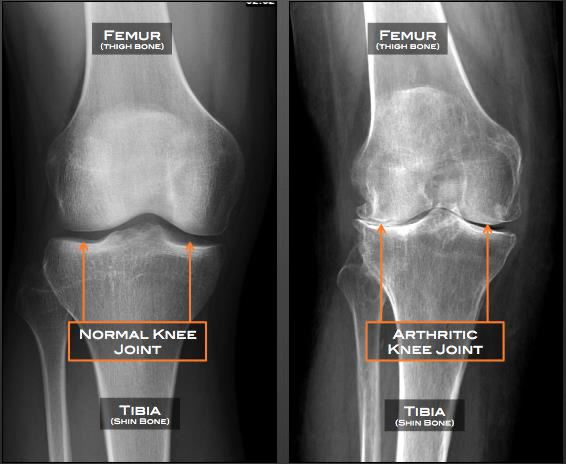
Knee X-ray of a normal (left) and an osteoarthritic (right) knee. Note the reduction in space between the two bones.
Diagnostic Ultrasound for Knee osteoarthritis
Many symptoms associated with osteoarthritis are caused by synovitis. Synovitis does not show on x-ray, but can be assessed using diagnostic ultrasound imaging. Diagnostic ultrasound can also highlight joint effusion, a reduced joint space, a Baker’s cyst and bony changes at the joint margins, which are also associated with OA.
MRI for Knee osteoarthritis
An MRI uses radio waves and a strong magnetic field to create images of both hard and soft tissues in your body. An MRI can sometimes be useful to assess for additional soft tissue problems, meniscal/cartilage tears and loose bodies in the knee, that often coexist with OA.
How Do We Treat Knee Osteoarthritis?
Unfortunately, it is not feasible to reverse the degenerative changes caused by osteoarthritis. However, it is possible to manage this condition using both physiotherapy and exercise and improve your pain.
At Complete Physio we offer a “one stop knee OA clinic” where we can provide a range of treatments to get people out of pain and back to full function. These include:
- Physiotherapy and guided rehabilitation
- Knee brace fitting
- Ultrasound guided injection therapy
This unique combination of treatments can provide excellent improvement in pain and function and reduce or delay your requirement for a total knee replacement or other surgery.
Physiotherapy and Guided Rehabilitation for Knee osteoarthritis
Physiotherapy treatment aims to improve the symptoms of the disease (i.e. knee pain, swelling, stiffness), and you should begin to notice a positive difference within a few physiotherapy sessions.
The main goals of physiotherapy for your knee arthritis are:
- Reduce your knee pain and inflammation.
- Normalise your knee joint range of motion.
- Strengthen your knee – especially your quadriceps and hamstrings.
- Strengthen your whole lower limb – calves, hip and pelvis muscles.
- Improve your patellofemoral (kneecap) alignment and function.
- Normalise your muscle lengths.
- Improve your proprioception, agility and balance.
- Improve your technique and function, e.g. walking, squatting, climbing stairs.
Your highly experienced physiotherapist will take you through a specific, tailored, rehabilitation programme, which may include:
- Relative rest – advice on rest and how you can modify your activity to allow the pain and inflammation in your knee to settle.
- Patient education – it’s important to understand your condition and to take an active role in your recovery. You will be given a clear explanation of the diagnosis and the causes of your symptoms, and we will discuss what is required to ensure you reach your goals.
- Pain and swelling management – Ice can be applied to the affected area to help with pain and swelling. Painkillers and anti-inflammatory medication are often useful in the early stages of management (any medication needs to be approved by a pharmacist or doctor).
- Acupuncture – this can be highly effective in helping treat pain and swelling around the knee.
- Range-of-movement exercise – your physiotherapist may teach you active range of movement and self-stretching exercises. These can decrease stiffness and help restore normal movement of your injured joints.
- Manual therapy – your physiotherapist may use manual therapy such as joint mobilisations, massage or soft tissue release techniques to the surrounding muscles. This will help improve joint movement and reduce muscle stiffness or soreness.
- Specific strengthening exercises – the muscles around your knee will need to be strong in order to help reduce the pressure going through your joint. Your physiotherapist will design a safe resistance program to ensure all your muscle groups (especially your quadriceps, hamstrings, glutes, and calves) are strong and working in synergy, to aid your recovery. You will be given exercises to continue independently; this is a key component of your treatment programme and will require some commitment and consistency.
- Proprioception and balance exercises – these exercises help your brain to reconnect with your knee, so that you know where your knee is in space and in relation to other parts of your body during movement.
- Biomechanical and movement re-education – this may involve teaching you how to correctly walk, squat, kneel, run, and/or any other specific activity.
- Functional and sports specific training – once your pain, strength, and range of movement improve, functional training can help you safely resume more demanding activities and sports.
Throughout your treatment at Complete Physio, we will ensure that you feel well supported and involved in your rehab. As part of the rehabilitation program, we also conduct regular clinical testing to ensure that you are on track with your recovery to achieve your goals.
Knee braces for Knee osteoarthritis
Your physiotherapist may recommend using a knee brace to support your knee and help off-load certain structures, particularly if only one compartment is affected i.e. unicompartmental OA. There are many different types of brace available, and it is important to find one that suits your individual needs. At Complete physio we have a specialist bracing service and recommend the Ossur Offloader.
Ultrasound guided injections for Knee osteoarthritis
If your pain is not well controlled, and physiotherapy is not helping, an ultrasound guided steroid injection can provide effective pain relief. Injections should always be followed up with a course of physiotherapy; they provide a window of opportunity to allow you to engage better with your rehabilitation.
Hyaluronic acid and PRP injections can provide an alternative to steroid injections and have been shown to be effective. They are reserved for mild to moderate knee osteoarthritis in active individuals.
Will I need knee surgery for Knee osteoarthritis?
If you have osteoarthritis that causes severe pain or has a significant impact on your daily life, and you have already tried the treatments mentioned above without the desired effect, your doctor may suggest you have surgery.
There are a number of different surgeries that might be effective in the treatment of knee OA. These include:
- Knee Arthroscopy – your surgeon may suggest you have keyhole surgery, particularly if your knee has been locking or if, for example, the symptoms might be due to a specific meniscal lesion rather than the coexisting OA.
- Cartilage Grafting – this might be an option for younger patients who have small areas of cartilage damage. Healthy cartilage is used to fill a hole in the cartilage of your bad knee.
- Knee Osteotomy – this procedure is done if just one side of the knee joint is damaged. Either the tibia (shinbone) or femur (thighbone) is cut and reshaped. This helps shift weight off the damaged side of the joint and can relieve pain and improve function.
- A Partial or Total Knee Replacement – your surgeon removes the damaged cartilage and bone, and then puts in new metal or plastic joint surfaces to reduce the pain and restore the function of the knee.
At Complete Physio we work with some of London’s most highly regarded and experienced orthopaedic surgeons. If an onward referral is required, we will ensure that you are provided with the best care possible, and will continue to support your recovery every step of the way.
After surgery you’ll be referred back to your physiotherapist at Complete for a course of post-operative rehabilitation to make sure you achieve the best outcome.
If you would like to book an appointment or speak to one of our expert physiotherapists about your knee, please call 020 7482 3875 or email info@complete-physio.co.uk.
Don’t let pain hold you back, book now!






