What Is Patella Tendinopathy?
Patellar tendinopathy (also known as jumper’s knee and patella tendinitis) is a common soft tissue injury which causes significant pain in the tendon on the front of the knee, below the knee cap (known as the patella). It can also cause stiffness and weakness around the knee. The pain is particularly noticeable in the morning and getting up after sitting for a while, for example, after driving or sitting in a cinema.
It is sometimes called ‘jumper’s knee’ because the injury often happens during sports that involve jumping, such as volleyball, netball or basketball . However, even people who don’t participate in jumping sports can get patellar tendinopathy. It is also common in football and cross-fitters.
The patellar tendon works with the muscles at the front of your thigh (quadriceps) to straighten your knee so that you can kick, run and jump. Patellar tendinopathy occurs when the patellar tendon is overused /overloaded. The tendon struggles to cope with the pressure put upon it resulting in micro-injuries and weakening of the structure; this causes swelling of the tendon and consequently pain. The process can occur over many months or can happen rapidly with one bout of intense exercise.
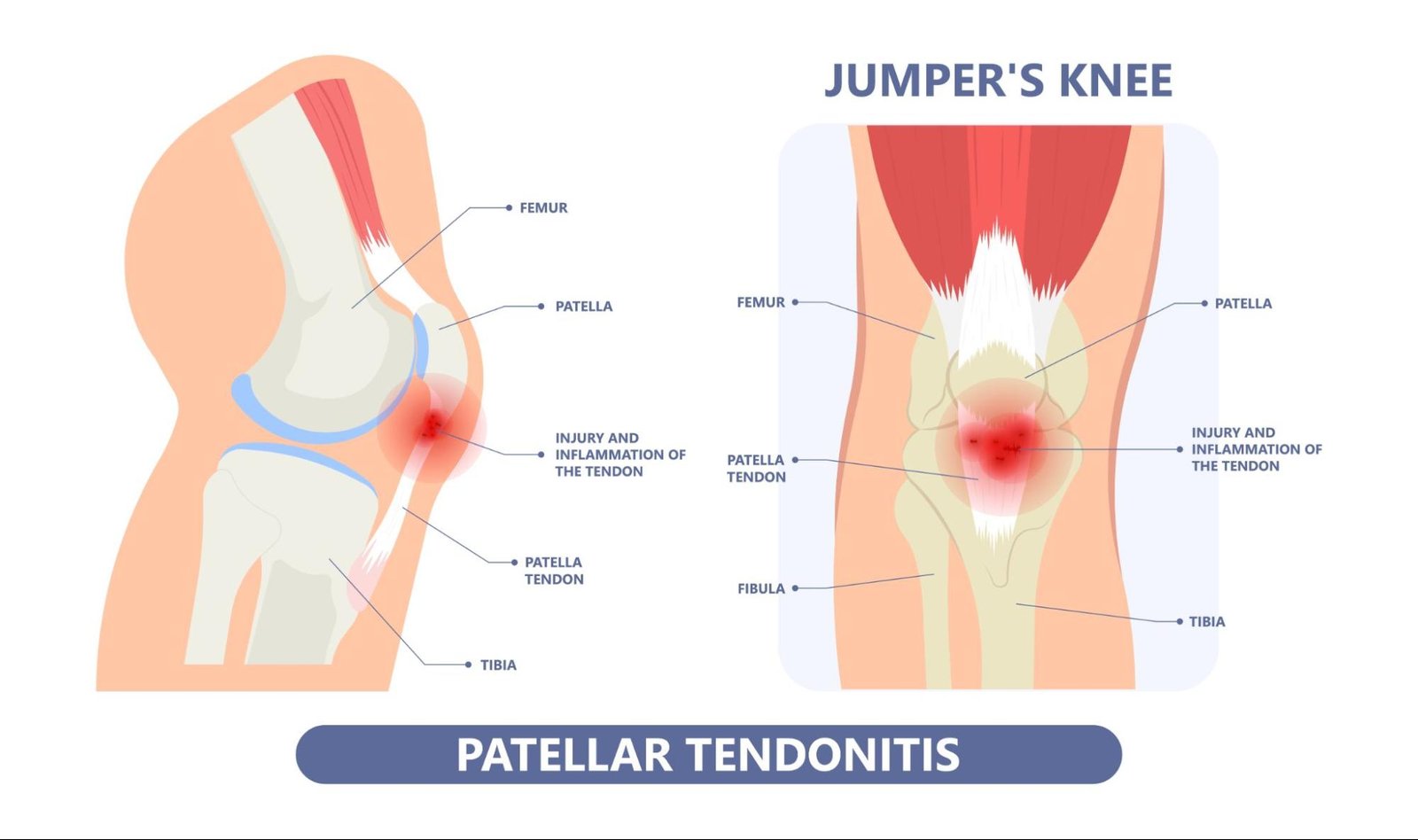
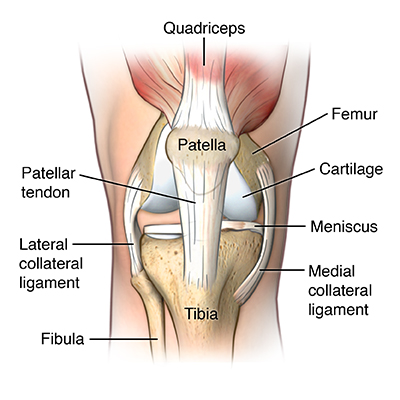
Anatomy of Patella Tendinopathy
The patella tendon is located just below the patella (knee cap), and it has attachments on the patella and the tibia (shin bone). The role of the patella tendon is to transfer the force of the quadriceps muscles via your patella and your upper tibia.
The quadriceps muscles, quadriceps tendon, patella and patellar tendon are responsible for extending (straightening) your knee during running and jumping and are collectively known as the knee extensor mechanism.
Your quadriceps are even more critical when controlling your knee as you bend from a straight position, e.g. walking down stairs and landing from a jump. Your quadriceps muscles are heavily involved in most sports, especially jumping, running and kicking.
Typically, patella tendon injuries occur in two areas:
- Proximal insertion of tendon – just below the kneecap where the tendon joins the muscle in the lowest point of the knee cap (patella). This is the most common region of pain i.e., on the tip of the knee cap.
- Distal insertion of tendon – where the tendon joins into the tibia (shin bone)
What Causes Patella Tendinopathy?
The role of a tendon is to withstand high, repetitive loading; however when the patellar tendon is subjected to excessive, high-intensity activity involving jumping, running or other heavy load, it can place excessive strain on the patella tendon.
When tendons become strained, they sustain small micro-tears, which causes inflammatory chemicals and swelling (tendonitis); quickly healing if managed appropriately with rest i.e. a reduction of the high impact forces. However, repeated bouts of overstrain to your tendon causes increased microtrauma. This ongoing trauma occurring in the tendon can exceed the rate of repair, resulting in an incomplete, sub-optimal healing response. At first, the damage may only be minor and not cause any problem, but damage will progressively become worse, causing the tendon to become more inflamed and thickened, which results in significant pain and dysfunction. This is patellar tendinopathy and in severe cases can result in larger tears or even tendon rupture.
This injury usually happens gradually over time. Researchers in this field still have unanswered questions about how or why patellar tendinopathy occurs, but there appear to be two main types of issues:
- Problems with tendon loading – sudden changes in tendon loading. Such as starting to train at the beginning of a sports season or increasing your running training too quickly. This type of tendinopathy is more common in patients aged 15-30. Men are also more likely to be affected.
- Problems with the health of the tendon – this usually affects older adults (over 35) as their tendons degenerate and become more rigid and stiff. This is part of the normal ageing process due to wear and tear. Genetics, smoking and some medical conditions can also affect the health of the patella tendon.
Risk Factors for Patella Tendinopathy?
A combination of factors may contribute to the development of patellar tendinopathy, including:
Training/activity level
This can occur in a variety of ways. For example:
- A rapid increase in the amount of training – how often you are training/playing.
- A sudden increase in training intensity – how hard and long you are training/playing for.
- Poor technique – If the way you are running/jumping/landing is not correct, you could put increased pressure through your patella tendon.
- Training/playing on rigid surfaces – this will cause increased impact going through the patella tendon.
Poor Flexibility
Tight quadriceps and/or hamstring muscles can increase the strain on your patellar tendon
Lower Limb Biomechanics
Biomechanical issues can include muscle imbalances, poor foot posture, structural abnormalities, or poor knee or hip control.
Your physiotherapist will assess this and treat these issues as required. Changing your footwear can also contribute to the
Chronic illness/health
Some illnesses disrupt blood flow, which can cause weakness in the tendons around the body (including the patella tendon). Examples include kidney failure, autoimmune diseases such as lupus or rheumatoid arthritis and metabolic diseases such as diabetes.
Patella tendinopathy has also been associated with a high body mass index (BMI) or sudden weight gain.
What are The Symptoms of Patella Tendinopathy?
The main symptom of patellar tendinopathy is pain, or aching, just below your kneecap. You’ll probably start to notice a gradual increase in pain, rather than having an injury that suddenly causes it. When you first feel pain, it will probably only come on after you exercise. As time goes by you may feel pain during exercise, which gets less after you warm up. This may then develop into constant pain for the duration of the activity. As well as being painful, your knee may be tender to the touch.
Symptoms often present gradually, without trauma, and can take weeks or months of repetitive overloading before becoming problematic. They can also come on more quickly if you have suddenly upped your training/activity level.
If you don’t have treatment for patellar tendinopathy, there’s a possibility that your tendon will eventually tear or rupture. If this happens, you may have sudden pain and your knee may give way.
Common Signs and Symptoms of Patella Tendinopathy:
- Pain/dull ache over the front of the knee below the knee cap.
- Pain is made worse with jumping, landing or running activity.
- Pain with negotiating stairs and inclines.
- Localised tenderness over the patella tendon (painful to touch)
- Often the tendon feels very stiff first thing in the morning or after periods of rest such as rising from sitting at your desk.
- Delayed pain that comes on sometime after a period of activity.
- The affected tendon may appear thickened in comparison to the unaffected side
If you are experiencing any of these symptoms in your knee, please book an appointment to see one of our expert physiotherapists. You can call 0207 482 3875 or email info@complete-physio.co.uk. If you would like to speak to a specialist before booking, then please email us with your details and we will call you back to discuss the best course of action.
How is Patella Tendinopathy Diagnosed?
It is essential to get an accurate diagnosis of your problem to ensure that you are started on the best and most effective treatment plan. Physiotherapists are highly skilled diagnosticians; your Physiotherapist will carry out a comprehensive subjective and clinical assessment. It is unlikely that you will need to have a scan prior to seeing a physio.
At your initial appointment your Physiotherapist will ask questions about your past health, symptoms, and exercise regime. This will help to build up a picture of what is likely to have caused/be the problem.
After your consultation, the specialist will complete a series of clinical tests to confirm their diagnosis; this may include:
- Assessing the range of movement of your knee joint, and strength of your lower leg muscles.
- Assessing muscle length and flexibility of calves, quadriceps, glutes and hamstrings
- Watching you move your knee and how you perform activities such as squatting, hopping, jumping, running.
- Checking other regions of the body as needed; such as hips, feet and lower back. This will help to determine if other areas are contributing to the problem, and also require treatment to improve your condition.
- Gently, but skilfully, feeling around your knee joint and patella tendon to find exactly where it is most painful.
The clinical assessment is normally sufficient to diagnose a patella tendinopathy, although it is not likely to identify a tear in the tendon.
If your symptoms are severe, or want to know if you have torn the tendon a diagnostic ultrasound scan is recommended.
X-Ray for Patella Tendinopathy?
An X-ray will not help to diagnose a tendon problem as soft tissue does not show up on x-ray, however it will show any bony abnormalities or damage such as osteoarthritis or bone fractures.
Diagnostic Ultrasound Scan for Patella Tendinopathy?
A diagnostic ultrasound scan is able to assess the tendon structure and inflammation associated with tendinopathy. Ultrasound is regarded as the gold standard imaging technique for assessing tendon structure and pathology, better than MRI.
A scan will be able to answer the following:
- How severe the tendinopathy is.
- Whether there is a tear in the tendon.
- If there is involvement of other structures such as the fat pad, bursa or meniscus (soft cartilage in the knee).
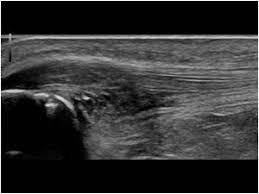
Ultrasound scan showing a significant patella tendinopathy
At Complete we are able to offer an ultrasound scan as part of your clinical assessment. There is no requirement to have a GP referral, and we do not charge extra for it. You will need to be booked in with one of our Clinical Specialists, so please ensure you inform our administration team at the time of booking.
To book an appointment to see one of our clinical specialists please call 0207 482 3875 or email info@complete-physio.co.uk.
MRI for Patella Tendinopathy?
An MRI scan is not required for diagnosing patella tendinopathy. MRI is a static test performed at rest with your knee straight. An MRI visualises the deeper structures in the joint better than ultrasound, such as the articular cartilage on the joint surfaces and it will pick up tears in the meniscus or cruciate ligaments.
Treatment for Patella Tendinopathy?
Physiotherapy and Rehabilitation for Patella Tendinopathy?
Patella tendinopathy is notoriously challenging to rehabilitate and therefore it is essential that treatment starts as early as possible. Rehabilitation requires specialist physiotherapy intervention, tailored to your specific needs to get you back to full function.
Complete Physio has gained an excellent reputation amongst patients and peers for providing a first class, highly specialised clinic for those suffering with tendon pain, particularly tendon pain which is not improving with conservative care. We treat elite and recreational athletes, from Professional footballers to Park Runners, but also those who lead a more sedentary lifestyle. We are trusted by world renowned orthopaedic surgeons and sports medicine consultants to treat their patients.
Your physiotherapist at Complete will provide you with a tailored regime based on your personal profile. This will often include:
- Relative rest – advice on rest and activity modification allowing the pain to settle and the patellar tendon to heal appropriately.
- Patient education – We will ensure that you have a clear understanding of your condition and what will be required to progress and optimise your recovery.
- Pain management – taping the knee to offload and reduce the pressure on the tendon can help to reduce your pain. Ice can also be applied to the affected area.
- Specific loading exercises – clinical research has shown that heavy slow resistance (HSR) exercises can have a positive effect on patellar tendinopathy. This is a key component of your treatment programme and requires commitment and consistency.
- Biomechanical and movement re-education – this may involve teaching you how to correctly squat, lunge, run or jump.
- Range-of-movement exercise – Your physiotherapist may teach you self-stretching methods. These can decrease tension and help restore normal motion of your injured joints.
- Manual therapy – In order to help improve movement and reduce muscle stiffness your physiotherapist may use manual therapy such as massage or soft tissue release techniques to the surrounding muscles.
- Muscle strength – muscle imbalances and weakness in the muscles of the lower limb can cause or contribute to problems with the patella tendon. Your physiotherapist will design a safe resistance program to ensure all your muscle groups are strong and working in synergy. This will help to aid your recovery and prevent recurrence of injury.
- Functional and sports specific training – once your pain, strength, and range of movement improve, functional training can help you safely resume more demanding activities and get you back to playing the sport that you love.
Shockwave Therapy – also known as Extracorporeal Shockwave Therapy (ESWT) for patella tendinopathy
Physiotherapy will always be the key component of any patella tendinopathy treatment pathway, but there are other options alongside physiotherapy to improve your pain and help the tendon to heal . Shockwave therapy compliments your rehabilitation programme and can significantly reduce your pain and speed up your recovery.
Shockwave therapy produces a series of powerful sound waves which provide a small dose of controlled microtrauma to the patella tendon. Research has shown that shockwave stimulates the tendons natural healing process, initiating a new healing process. Local nerve endings surrounding the painful tendon become desensitised by these pulses, resulting in pain and symptom reduction.
Recent evidence suggests positive outcomes following 3-5 shockwave treatment sessions running concurrently with a progressive loading exercise program for the treatment of all lower limb tendinopathies. For more information about shockwave therapy click here.

Complete Physio’s tendon specialists have shockwave therapy available at three of our clinics. Shockwave is available at our Bury Street (next to Gherkin), Chelsea and Angel clinics.
Injection therapy for patella tendinopathy
If your pain has persisted for over 3 months and you have not improved with physiotherapy then you may be appropriate for injection therapy. Injection therapy is used within musculoskeletal medicine to reduce pain and inflammation, allowing you to effectively rehabilitate your condition.
There are three injection options for patella tendinopathy.
1. Ultrasound-guided high-volume injection
An ultrasound-guided high-volume injection uses a combination of saline (sterile water) and a local anaesthetic to reduce pain. This technique has been practised for over 10 years and has good evidence to support its use. The injection uses a high volume of saline to ‘strip’ the tendon away from the underlying fat pad (known as Hoffa’s fat pad). This helps the tendon to heal, reduces any adhesions between these structures to improve the ‘sliding’ of the structures on each other.
2. Ultrasound-guided platelet-rich plasma (PRP) injection
PRP has been clinically proven to enrich the healing process and speed recovery of tendons. It is a natural, safe treatment for patellar tendinopathy using components of your own blood to heal the tendon. There are very few side effects and the procedure is well tolerated. Although there is evidence to support its use in patella tendinopathy, it is reserved for cases that have failed to respond to all other treatment options.
PRP requires a small amount of blood to be extracted from a vein in your arm. Blood is then spun, at high speeds, in a centrifuge machine. This separates the PRP from other blood molecules. PRP is then injected, under ultrasound guidance, in and around the patellar tendon to target the most affected regions. If a tear is identified on ultrasound, it will be directly injected into the tear to facilitate the healing process.
Research suggests that a series of three injections is required to successfully treat tendinopathic pain.
3. Ultrasound-guided hyaluronic acid injection
Hyaluronic acid is a naturally occurring substance that can be used in stubborn cases of patella tendinopathy. It is not placed into the tendon directly but around the tendon between the tendon and Hoffa’s fat pad. This helps to improve the gliding of the tendon and reduce the pain. Hyaluronic acid also has some anti-inflammatory properties and is now being used as a safer and longer-acting alternative to steroids. It also has the added benefit of being nourishing for the joint so aiding the preservation of joint surfaces and thus longevity of the joint.
A hyaluronic acid injection for patella tendinopathy is a one-off injection.
Throughout your treatment, your Physiotherapist will keep revisiting your personal goals, ensuring that you feel supported and have an active involvement in your recovery process. We are dedicated to getting you back to full function and all the activities that you enjoy.
Surgery for patella tendinopathy
Most people with patellar tendinopathy don’t need surgery. But it may be an option if your symptoms don’t improve with other treatments after three to six months, or if your tendon tears (ruptures).
The aim of surgery is to repair your tendon and it’s usually done in an arthroscopy procedure, which is a type of keyhole surgery. A physiotherapy guided rehabilitation programme will be needed following surgery to restore full movement and strength, and get you back to full activity.
If an onward referral is required, we will ensure that you are provided with the best care possible. We work with some of the best and most experienced surgeons in the country, and we will continue to support your post op recovery every step of the way.
If you would like to book an appointment or speak to one of our expert physiotherapists please call 020 7482 3875 or email info@complete-physio.co.uk.
Don’t let pain hold you back, book now!





