What is patellofemoral pain syndrome (PFPS) – also known as patellofemoral joint pain or anterior knee pain?
Patellofemoral pain syndrome is the medical term used for pain felt at the front of your knee, behind your kneecap, or around your kneecap. It is caused as a result of stress on the joint where your patella (kneecap) articulates with your thigh bone (femur). This joint is known as your patellofemoral joint.
Patellofemoral joint pain is one of the most common knee complaints of both the young active sportsperson and the elderly. In the younger population, it is usually caused by muscle imbalances or altered lower limb mechanics, which results in patellofemoral joint irritation and pain. In the older population, it is usually due to longstanding ‘wear and tear’ on the joint which damages the cartilage and joint surfaces and can cause osteoarthritis.
It is more common in females than males and is often aggravated by prolonged walking, particularly downstairs or down hills, squatting, lunging, and running. In most cases, pain increases with activity or after sitting for long periods of time with the knees bent. It can affect one or both knees.
Sometimes you may hear the condition being referred to as chondromalacia patella, patella maltracking, or anterior knee pain.
Knee and Patellofemoral Joint Anatomy
The patellofemoral joint (PFJ) is where your kneecap (patella) and the thigh bone (femur) meet at the front of your knee. Patellofemoral ligaments connect the patella to the femur. The underside of your kneecap sits in a groove in the thigh bone called the trochlea that allows the patella to glide up and down smoothly as the knee bends and straightens. The kneecap can also make small side-to-side, tilting and rotation movements.
When you contract the muscles on the front of your thigh (quadriceps) they pull on the tendon that attaches to your kneecap. This allows your lower leg to straighten. This contraction, with the addition of a number of other muscles, allows the kneecap to glide securely in the groove during motions such as walking and climbing stairs. The strength of these muscles is essential for the normal mechanics of the joint. Weak muscles may result in pain and inability to carry out activities such as squats, going downstairs and running.
A layer of articular cartilage covers the ends of the femur, the trochlear groove, and the underside of the patella – the bone surfaces that make up the PFJ. Articular cartilage provides a smooth surface, reducing friction on the bones during movement.
What causes patellofemoral pain syndrome?
Many things may contribute to the development of PFPS. Problems with the alignment of the kneecap and overuse from vigorous sports or training are often significant factors.
Common causes of PFPS are:
- Overuse – running or jumping sports puts repetitive stress on your patellofemoral joint, which can cause irritation under the kneecap.
- Muscle imbalances or weaknesses – patellofemoral pain can occur when the muscles around your hip and knee do not keep your kneecap properly aligned or supported in the trochlea groove. In more extreme cases this can cause patellofemoral instability/dislocation, i.e., when the kneecap ‘slips’ out of the groove it is supposed to sit in. This is very painful if it occurs.
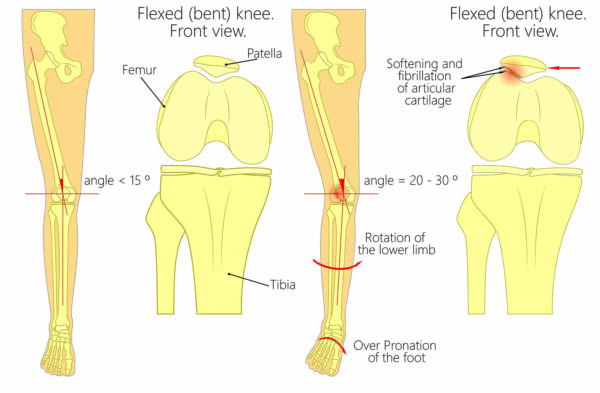
- Poor foot biomechanics – excessive pronation (flat foot) can result in increased pressure through the patellofemoral joint (see image below).
- Bony abnormality – if your kneecap is shaped differently, is situated particularly high on your knee (known as “patella alta”), or if there is a bony defect affecting your kneecap, this may cause patellofemoral pain.
- Lower leg alignment – this can have an effect on patellofemoral alignment, whether due to muscle imbalances, or the specific shape of the bones (such as ‘knock knees’ or ‘bow legs’). This ‘malalignment’ can potentially lead to an uneven distribution of load across the joint, putting too much stress on one area, resulting in pain.
- Injury – trauma to the kneecap, such as a dislocation or fracture, has been linked to patellofemoral pain syndrome.
At Complete Physio we are experts in treating all knee complaints, including patellofemoral pain syndrome. If you would like to book an appointment or speak to one of our physiotherapists before making a booking, please email info@complete-physio.co.uk or call 020 7482 3875.
Risk factors
Age – patellofemoral pain syndrome typically affects adolescents and young adults. Knee problems in older populations are more commonly caused by osteoarthritis.
Sex – women are twice as likely as men are to develop patellofemoral pain. This may be because a woman’s wider pelvis increases the angle (known as the Q angle) at which the bones in the knee joint meet.
Certain sports – participation in running and jumping sports can put extra stress on your knees, especially when you increase your training level.
What are the symptoms of patellofemoral pain syndrome?
The most common symptom of PFPS is a dull, aching pain in the front of the knee, which can increase to a sharper pain with certain activities. Symptoms can range in severity from mild to severe. It can affect one or both knees.
Patellofemoral pain symptoms typically present during weight-bearing or jarring activities that involve knee bending. Squatting, kneeling, hopping, running or using stairs (especially going downstairs) are commonly painful.
As your patellofemoral pain syndrome progresses, your knee may become painful while walking and then ultimately even at rest (particularly when sitting with knees bent).
Common symptoms include:
- Pain at the front of the knee, around and behind the kneecap
- Worsening pain during activity or exercise
- Pain after prolonged sitting
- Pain when squatting or going down stairs
- Clicking or grinding feeling in the knee
- Tender to touch on or around the knee cap
- Swelling over the front of the knee
If you are experiencing any of these symptoms or suspect that you have a patellofemoral joint injury and would like to see one of our expert physiotherapists, please call 020 7482 3875 or email info@complete-physio.co.uk. If you would like to speak to a specialist before booking, then please send us an email with your details and we will call you back.
How is patellofemoral joint pain diagnosed?
It is essential that an accurate diagnosis of patellofemoral pain syndrome is obtained. A diagnosis will be made by your physiotherapist by carrying out a comprehensive clinical assessment. It is not essential at this stage to have a scan.

They will ask questions about your past health, symptoms, and exercise regime to assist making a diagnosis.
After the history is taken, your specialist will complete a series of tests to further help develop a diagnosis. This may include:
- Measuring the range of movement of your knee.
- Assessing muscle strength, specifically the quadriceps in your knee and also the muscles around your hips.
- Looking at the alignment of your pelvis, hips, knees and feet.
- Assessing muscle length and flexibility of quadriceps and hamstrings.
- Examination of the position and alignment of the knee cap.
- Watching you move your knee and how you perform activities such as squatting, hopping, jumping, running.
- Gently, but skilfully, feeling around your knee joint and patella to find exactly where it is most painful.
- Functional tests – if your pain is present during a specific activity or task, you may be asked to perform these, so the physiotherapist can assess exactly what is aggravating your pain.
X-ray
If your clinician suspects the presence of cartilage damage (osteoarthritis) you may be referred for an x-ray. X-ray is regarded as a gold standard imaging technique capable of accurately diagnosing the presence and severity of bone and joint pathology, including osteoarthritis. It can also show the alignment of the kneecap.
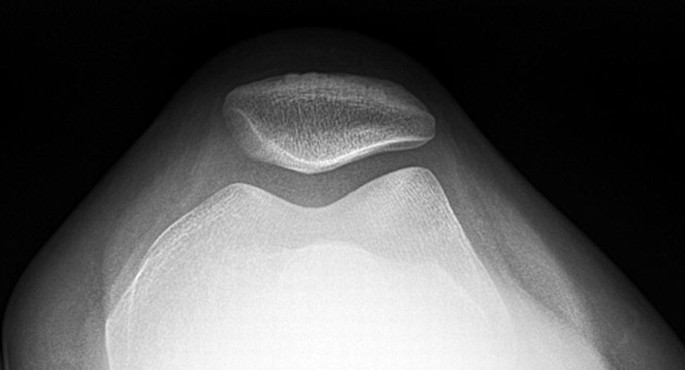
Image of a normal patellofemoral joint space and alignment
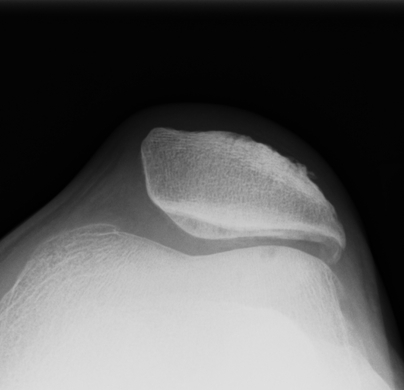
Image of patellofemoral malalignment and reduced joint space
Diagnostic Ultrasound
Diagnostic ultrasound imaging has been shown to be a highly effective imaging tool for visualising factors associated with patellofemoral knee joint pain. It is capable of detecting early-stage wear and tear within the trochlear groove. Ultrasound is also excellent at visualising swelling and inflammation of the joint. Ultrasound can also help to assess for other causes of knee pain that cause similar symptoms to patellofemoral joint pain, such as patella tendinopathy.

At Complete our clinical specialists carry out an ultrasound scan as part of their clinical assessment. We do not charge extra for an ultrasound scan, and you do not require a GP referral. If you would like to book an appointment including an ultrasound scan, please ensure you inform our administration team at the time of booking.
To book an appointment with one of our clinical specialists, please call 020 7482 3875 or email info@complete-physio.co.uk.
MRI scan
An MRI scan is not usually required to diagnose patellofemoral pain syndrome but can be very useful for ruling out other causes of knee joint pain. If your symptoms are not improving and underlying pathology is suspected, your clinician may refer you for further investigations including an MRI. An MRI provides a good overview of all types of tissue – bone, cartilage, ligaments, muscle, tendon, bursae, and other structures – so can be very helpful in differentiating where the problem may lie.
How do we treat patellofemoral pain syndrome?
PFPS usually responds well to management with specific exercise and lifestyle changes. It is unlikely that surgery of any kind will be required.
Researchers have confirmed that physiotherapy intervention is a very effective short and long-term solution for patellofemoral pain.
Over 90% of patellofemoral syndrome sufferers will usually respond favourably to exercise-based treatment. Becoming pain-free within six to eight weeks of starting a physiotherapy guided rehabilitation program is commonplace. However, many factors will determine your rate of recovery, and your physiotherapist will guide you through the best treatment pathway for your individual needs.
Treatment aims to reduce your pain and inflammation in the short term and then, more importantly, address the underlying causes to prevent it from returning in the long term.
Your physiotherapist at Complete will provide you with a tailored regime based on your personal profile.
This will often include:
- Activity modification – advice on rest and activity modification, allowing the pain to settle.
- Pain management – taping the knee to offload and reduce the pressure on the kneecap can help to reduce your pain. Taping can allow you to carry out your physiotherapy exercises and everyday activities with less pain. Ice can also be applied to the affected area. You may also benefit from taking some anti-inflammatory medication.

- Patient education – it’s important to understand your condition and to be active in your recovery. You will be given a clear explanation of the diagnosis and any other underlying causes, and we will discuss what is required to address these issues and reach your goals.
- Range of movement exercises and muscle stretches – your kneecap and knee must be able to glide through its full normal range of motion. Your physiotherapist will assess your movement and apply the necessary techniques to normalise your joint and muscle range of movement. You will also likely be given range of movement and stretching exercises to do at home.
- Manual therapy – your physiotherapist may use manual therapy such as massage or soft tissue release techniques to the surrounding muscles. This will help improve movement and reduce muscle stiffness or soreness.
- Specific strengthening exercises – muscle weaknesses or imbalances throughout the lower limb can cause or contribute to problems with patellofemoral joint pain. Your physiotherapist will design a safe resistance program to ensure all your muscle groups are strong and working in synergy, to aid your recovery and prevent recurrence of injury. This is a key component of your treatment programme. The balance of muscle strength and control of your quadriceps is particularly important and will often be an area your physiotherapist will focus on. The balance of the quadriceps in relation to your other muscles such as your hamstrings and calf muscle is very important. Other muscle groups particularly around the hip such as the adductor and abductor muscles are also important to normalise kneecap mechanics.
- Biomechanical and movement re-education – this may involve teaching you how to correctly squat, run or jump. This will help to promote normal movement patterns and reduce the pressure on your kneecap. If there is an issue with your foot position and mechanics, i.e., if your foot overpronates, you may require a referral to a podiatrist for an orthotic (bespoke insole) for your shoe. There is good evidence in the scientific literature that orthotics can help to reduce patellofemoral joint knee pain and improve your function.
- Functional and sports-specific training – once your pain, strength, and range of movement improve, functional training can help you safely resume more demanding activities and get you back to playing the sport that you love and minimise your chance of future injury.

Throughout your treatment at Complete Physio, we will keep revisiting your personal goals, so that we maintain the focus on making your life easier and ensuring that you feel supported and involved in your rehab process. We are dedicated to getting you back to full function and we have the correct skills and knowledge within the practice to ensure this goal is achieved.
What do I do if my patellofemoral joint pain symptoms don’t improve?
If a course of physiotherapy and a progressive home exercise program has not sufficiently helped you, then an ultrasound guided injection may be appropriate.
Injection therapy is used to reduce pain and inflammation associated with the patellofemoral joint and can provide you with a ‘window of opportunity’ to effectively rehabilitate your knee in a pain-free environment.
Injection therapy is particularly helpful if you are suffering one or more of the below scenarios:
- Pain is affecting your ability to sleep or is waking you up at night.
- Pain is limiting your activities of daily living.
- Pain is affecting your ability to work or partake in leisure activities.
- Pain is limiting your ability to complete your physiotherapy programme.
All injections at Complete are carried out using ultrasound guidance. Ultrasound guided injections have shown high levels of accuracy, reduced post injection complications, and increased levels of pain relief when compared to injections performed without ultrasound guidance.
At Complete Injections our highly trained team of clinicians are qualified to perform ultrasound guided injections for patellofemoral knee joint pain. All clinicians are experienced physiotherapists, musculoskeletal sonographers, independent prescribers, and injection therapists who are able to perform a same day injection service on all guided injections. You can self-refer directly into our service. You do not need to see a GP first.
There are two ultrasound-guided injection options available for the treatment of patellofemoral joint pain:
Ultrasound guided corticosteroid injection
When undertaking a steroid injection, an ultrasound machine is used to accurately place the needle to deposit a combination of corticosteroid (powerful anti-inflammatory medication) and short-acting local anaesthetic directly to the source of your pain. A corticosteroid injection is an effective treatment for reducing pain and inflammation associated with patellofemoral pain syndrome. Steroid injections are reserved for those in severe pain.
Ultrasound guided hyaluronic acid injection
The hyaluronic acid injection technique uses a natural (non-drug) synthetic version of the joint’s natural lubricant. Hyaluronic acid has also been shown to have powerful anti-inflammatory properties and is regularly used as an alternative to corticosteroid for the treatment of patellofemoral pain syndrome. Hyaluronic acid injections are advised for those with moderate to severe pain.
Steroid and hyaluronic acid can also be injected together as a combination therapy.
Injection therapy should not be used as a stand-alone treatment. For the best, long-term results it is important that you use the pain relieving effects of the injection to commence a programme of physiotherapy within 2 weeks.
If you would like more information or would like to book an appointment, please contact us on 020 7482 3875 or email injections@complete-physio.co.uk.
Surgery for Patellofemoral Joint Pain
If non-surgical treatments aren’t effective, your specialist might suggest:
- Arthroscopy – during this procedure, the doctor inserts a pencil-thin device equipped with a camera lens and light (arthroscope) into your knee through a tiny incision. Surgical instruments are passed through the arthroscope to remove fragments of damaged cartilage.
- Realignment – in more-severe cases, a surgeon may need to operate on your knee to realign the angle of the kneecap or relieve pressure on the cartilage.
At Complete Physio we work with some of London’s most highly regarded and experienced consultants. If an onward referral is required we will ensure that you are provided with the best care possible, and will continue to support your recovery every step of the way.
If you would like to book an appointment or speak to one of our expert physiotherapists, please call 020 7482 3875 or email info@complete-physio.co.uk.
Don’t let pain hold you back, book now!





