
What is Piriformis Syndrome?
Piriformis syndrome is a fairly uncommon condition in which the piriformis muscle, located in the buttock region, causes buttock pain. The piriformis muscle compresses and irritates the sciatic nerve which can cause pain, numbness and tingling along the back of the leg and into the foot.
The piriformis can be a large generator of pain and also be very sensitive due to its close proximity with the sciatic nerve. It usually happens on just one side of your body, but can sometimes occur on both sides concurrently.
It is important to mention at this point that most buttock and leg pain is not due to piriformis syndrome and is far more likely to be related to your lower back or hip joint. The most common cause of buttock and leg pain is due to irritation of the sciatic nerve by a disc in the lower spine, more specifically the region known as the lumbar spine.
Anatomy of the Piriformis Muscle and Sciatic Nerve
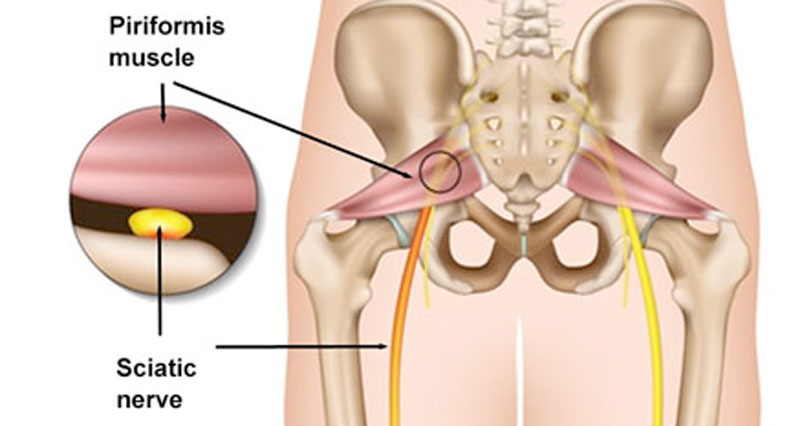
The piriformis muscle is a fairly small, flat, triangular shaped muscle, located deep in the buttocks near the top of the hip joint. It starts at the lower spine (sacrum) and connects to the upper surface of the femur (thighbone).
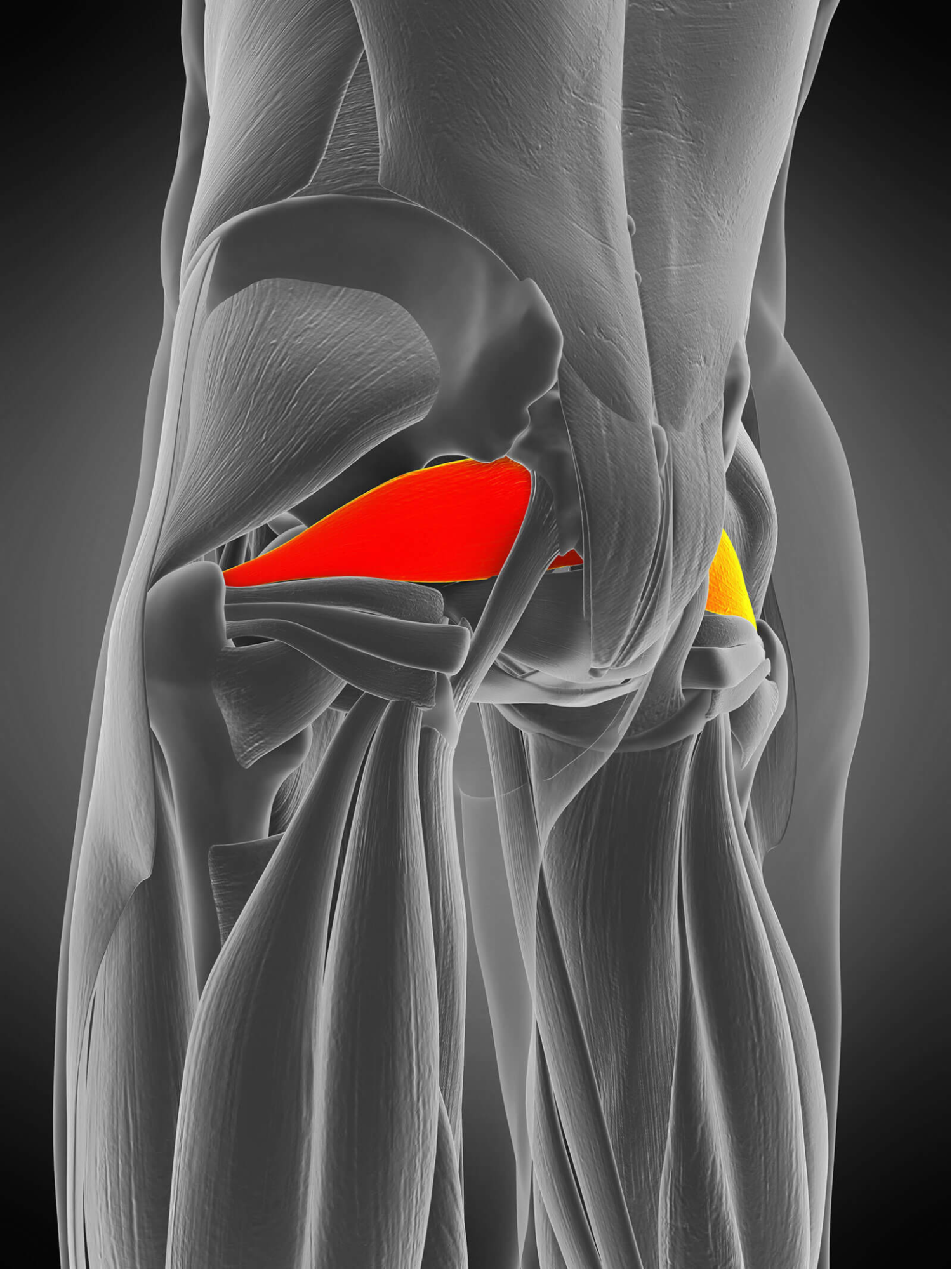
The piriformis muscle is important in almost all lower body movements. This is because it stabilises the hip joint, assists in lifting and rotating the hip and helps turn the leg and foot outward. This enables us to walk and maintain our balance as we shift our weight from one foot to the other.
The sciatic nerve is thick and is the longest nerve in the body. It travels from the spinal cord in your lower back and typically passes underneath, or, in some people, through the piriformis muscle. It then continues down the back of the leg and eventually branches off into smaller nerves that end in the feet.
What Causes Piriformis Syndrome?
Effectively, the cause of piriformis syndrome is a form of ‘sciatica’ which, insead of being generated by compression of the nerve root in the spine, is caused by compression of the sciatic nerve where it runs underneath, or next to the piriformis muscle.
The piriformis gets a workout every day; any movement or activity that requires us to stand or move our legs will activate our piriformis muscle. However when the muscle is overused or put under excessive stress or load, it can go into spasm.
Common Causes of Piriformis Syndrome:
- Rapid increase in training or activity level
- Long distance running
- Sitting for extended periods
- Heavy, repeated lifting – weight lifting or work related lifting
- Poor running technique
- Extensive stair climbing
- Muscle imbalances – such as tight adductors, or weak gluteal muscles
- Significantly unequal leg lengths – this would be considered > 1cm compared to the other side.
- Poor/abnormal spine alignment
What are the symptoms of Piriformis Syndrome?
A typical patient with piriformis syndrome complains of sharp, severe, pain in the buttock, with radiating symptoms down the back of the leg and into the thigh, calf, and foot. These symptoms often become worse after prolonged sitting, walking or running long distances, and may feel better when lying down on your back.
Common Symptoms Include:
- Pain in the buttock.
- Pain down the back of the thigh, calf and foot.
- Discomfort with prolonged sitting or putting weight on the buttock on one side.
- Pain when walking up stairs or inclines.
- Muscle spasm felt deep in the area of the piriformis muscle.
- Occasional pins and needles and numbness in the lower leg or foot.
- Tenderness with pressing on the muscle, and a reproduction of pain.
How is Piriformis Syndrome Diagnosed?
Piriformis syndrome is very difficult to specifically diagnose as the condition does not consistently show on MRI, ultrasound or X-ray. This makes getting an accurate diagnosis very challenging.
Therefore, piriformis syndrome is normally a diagnosis of exclusion, where all other conditions are ruled out. Piriformis syndrome mimics other, potentially more common conditions, such as intervertebral disc issue, sacral joint dysfunctions, trochanteric bursitis, femoroacetabular impingement and proximal hamstring pain.
A quick and accurate diagnosis is vital in order to ensure the condition does not lead to more chronic dysfunction and compensatory changes. Our physiotherapists at Complete Physio are highly skilled diagnosticians, who will be able to assess and recognise signs and symptoms that are unique to piriformis syndrome, therefore enabling the best and most appropriate treatment.
Clinical Examination
At your initial assessment your expert physiotherapist will take you through a clinical interview, to build up a picture of your pain and symptoms. They will ask questions about your past health, progression of symptoms and what aggravates and eases your pain, as well as what your normal daily activities and exercise routine is.
After your consultation, the specialist will complete a series of clinical tests and a physical examination to help develop a diagnosis. This may include:
- Range of movement testing of your spine and hips.
- Measuring the strength, length and flexibility of your lower limb muscles.
- Assessing your posture.
- Measuring leg length.
- Looking at functional movements such as squatting, balancing, lunging, stepping.
- Gait (walking or running) analysis.
- Neurological testing of the sciatic nerve.
This process is often all that is required to make a diagnosis of piriformis syndrome. However where symptoms are chronic or if the diagnosis is still unclear, specialist imaging/scans may be required to fully confirm the diagnosis and exclude other causes or pathology.
Diagnostic Imaging
X-ray


An X-ray shows bone and joints rather than soft tissue, therefore it is generally not used to diagnose piriformis syndrome,. However, it can be very useful in ruling out other causes of pain, such as stress fractures, hip or lumbar spine joint pathology, that can mimic piriformis syndrome.
MRI – Magnetic Resonance Imaging

An MRI uses radio waves and a strong magnetic field to create detailed, 3D images of both hard and soft tissues in your body. An MRI can visualise the piriformis muscle and sciatica nerve clearly but cannot consistently visualise the sciatic nerve as it travels next to the piriformis to detect inflammation and compression.
If appropriate, we can refer you directly for an MRI without going to your GP.
Diagnostic Ultrasound Imaging
Diagnostic musculoskeletal ultrasound is an excellent imaging tool for assessing soft tissue pathology around the hip and gluteal muscles. An MRI scan is able to clearly visualise the piriformis muscle and the sciatica nerve. However, cannot detect inflammation or compression of the sciatic nerve as it travels alongside the piriformis
The advantage of ultrasound, over an MRI, is it can assess the structures dynamically, which means that the scan can be carried out during the specific movement that causes your pain.
At Complete we have a unique team of specialist clinicians who can carry out an ultrasound scan as part of their clinical assessment. We do not charge extra for an ultrasound scan, and you do not require a GP referral.
If you would like to book an assessment with one of our clinical specialists, including an ultrasound scan, please ensure you inform our administration team at the time of booking.
To book an appointment to see one of our clinical specialists please call 0207 482 3875 or email info@complete-physio.co.uk.
How do we treat piriformis syndrome?

Physiotherapy for Piriformis Syndrome
Piriformis syndrome can be treated effectively with physiotherapy.
At Complete Physio we are highly experienced in treating soft tissue problems and your physiotherapist will take you through a personalised, progressive treatment and rehabilitation program to ensure you fully recover from your symptoms.
Physiotherapy treatment will often involve:
- Patient Education – You will be given a clear explanation of the diagnosis as understanding your condition will help you feel reassured and also more engaged in your recovery process.
- Modification of Exercise and Training – You will likely need rest and reduce your activity schedule to allow pain and inflammation to settle and the nerve and muscle to heal appropriately.
- Advice on Pain Management – Ice can be an excellent modality to help control pain, inflammation and swelling. You may also benefit from discussing pain medication or muscle relaxants with your GP.
- Acupuncture – Traditional acupuncture and dry needling techniques can be used to desensitise the sciatic nerve and also help to reduce muscle tightness and spasm.
- Focused Strengthening Exercises – Your physiotherapist will design a personalised, safe, progressive, resistance program to ensure all your lower limb muscle groups are strong and working in synergy. This will focus specifically on exercises for the hips and gluteal region, and supporting muscles.

- Core Stability – You will also need to work on your core stability as it is vital to have a strong centre in order to move your limbs effectively and efficiently. These are often Pilates based exercises, which strengthen your deep core muscles.
- Stretching Exercises – For key lower limb muscles – glutes, adductors and abductors. You may also be given some gentle stretches for the sciatic nerve to help to desensitise it and reduce neural tension.
- Hands-on Treatment – Your physiotherapist may use massage or trigger point release techniques to the piriformis and surrounding muscles to help reduce muscle stiffness and soreness. Foam rollers and massage balls are an excellent way to help release the piriformis as part of your home exercise programme.
- Running Gait analysis – Your physio may assess your running and teach you how to correct your technique so that you are activating the correct muscles and moving more efficiently, without aggravating your symptoms.

- Movement re-education and Sports Specific Rehabilitation – Once your pain, strength, and range of movement improve, functional training will ensure that you are able to resume more demanding activities and get you back to doing the sport that you love.
At each treatment session your Physiotherapist will continue to monitor your progress and revisit your personal goals, so that we ensure you feel supported and involved in your rehabilitation process. We are dedicated to getting you back to full activity and function and we have a highly skilled team of practitioners to ensure your goals are achieved.
Physiotherapy should always be the key component of your piriformis syndrome treatment pathway, but there are other options alongside physiotherapy which can improve your pain and help the muscle to heal.
What if My Pain and Symptoms Don’t Improve?
If physiotherapy treatment has not effectively reduced your pain and symptoms, and you have an accurate diagnosis of piriformis syndrome from diagnostic imaging, then an ultrasound-guided injection may be the next appropriate step for you.
Ultrasound-guided corticosteroid injection
Cortisone injections can be very effective, particularly if you are getting pain at night, or you are not able to take part in normal daily activities, or engage in your physiotherapy, due to your pain and symptoms.
Ultrasound-guided corticosteroid injections can be an effective, evidence-based treatment option for persistent pain associated with piriformis syndrome.
During an ultrasound-guided injection, a needle is accurately placed into the piriformis muscle and a combination of anti-inflammatory medication (corticosteroid) and a short-acting local anaesthetic is injected. An ultrasound-guided injection should provide significant pain relief for at least 6–8 weeks which will allow you a window of opportunity to engage in your physiotherapy programme and prevent re-occurrence of your symptoms. Complete physio recommends that a course of physiotherapy starts no longer than two weeks after the injection to ensure optimum results.
At Complete all our clinicians are highly experienced and carry out ultrasound guided injections as part of their daily practice. We are able to provide a ‘one stop’ guided injection service.
You do not require a GP referral, and you do not need to bring a prescription with you. Your injection appointment includes a full and accurate assessment, diagnostic imaging, medication prescription, ultrasound-guided injection and a comprehensive clinical letter.
Surgery for Piriformis Syndrome
Piriformis syndrome surgery is rarely offered.
If you would like more information about piriformis syndrome or would like to make an appointment to get out of pain and back to full function, please call 020 7482 3875 or email info@complete-physio.co.uk.
Don’t let pain hold you back, book now!





