If you’re struggling with jaw pain, clicking, or tightness around your jaw and face, you might be surprised to learn that the root cause of the issue may not be your jaw at all – it could be coming from your neck.
The relationship between the temporomandibular joint (TMJ) and the cervical spine (neck) is complex and the connection is often overlooked.
In this blog, we’ll explore how the TMJ and cervical spine are interconnected, how posture plays an important part of diagnosis and treatment of TMJ dysfunction and what can go wrong when this balance is disrupted.
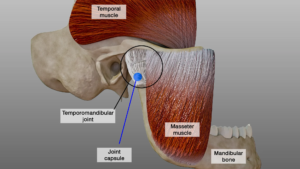
What is the TMJ?
The temporomandibular joint is the hinge joint that connects your jawbone (mandible) to the temporal bone of your skull, located just in front of your ears. You use this joint every time you talk, chew, yawn, or open your mouth. It’s one of the most frequently used joints in the body and relies on a delicate balance of muscles, ligaments, and bone positioning for smooth function.
When things go wrong, symptoms can include:
- Jaw pain or tightness
- Clicking, popping, or locking of the jaw
- Headaches
- Earaches or a feeling of fullness in the ears
- Tinnitus (ringing in the ears)
- Facial pain
- Neck stiffness
Anatomy of the Cervical Spine
The cervical spine consists of the top seven vertebrae in your spinal column (C1 to C7), supporting the skull and allowing for a wide range of head and neck movements.
Between each vertebrae are intervertebral discs which act as shock absorbers, and protect your neck joints. This shock absorbing mechanism also reduces the vibrations and forces going through your skull when we walk or run, helping protect your brain.
The cervical spine is much more mobile than the thoracic and lumbar spine, allowing you to move your head in nearly every direction. Unfortunately this level of flexibility often makes it more susceptible to injury.
The Link Between the Cervical Spine and TMJ Dysfunction
The cervical spine (neck) and temporomandibular joint (TMJ) are closely connected, both anatomically and neurologically.
In particular, dysfunction at the C2-C3 level of the spine can contribute to TMJ pain and movement restrictions. The upper cervical spine shares nerve pathways with the TMJ via the trigeminal nerve, meaning irritation or dysfunction at C2-C3 can lead to referred pain in the jaw, face, and even the ear.
Additionally, poor mobility or muscle imbalances in this area can alter postural alignment, increasing strain on the TMJ.
How does cervical spine dysfunction affect the TMJ?
When the cervical spine isn’t functioning properly, it can create a ripple effect that impacts your jaw mechanics.
Common cervical issues include:
- Stiffness or hypomobility: Limited movement in the neck joints, especially in the upper cervical spine, can alter your head position and muscle tension, which can impact the TMJ.
- Hypermobility: Excessive movement in the neck can cause instability around the spine, leading to your muscles having to overcompensate and become tight and overworked, increasing the tension in your jaw.
- Muscle imbalance or spasm: Overactive or underactive muscles in the neck and shoulders can pull the jaw into a misaligned position, contributing to TMJ pain.
- Forward head posture: A postural dysfunction where the head juts forward over the shoulders can increase the strain on both the neck and jaw structures.
The Posture Connection – Jaw, Neck and Shoulders
Your posture is a key player in the TMJ-cervical spine relationship. Poor posture, especially from prolonged, slumped sitting, mobile screen or TV use, or poor sleeping positions, can often lead to the following poor posture:
- Forward head, poking chin posture, which shifts the jaw backward into a compressed position.
- Rounded shoulders, which alters muscle recruitment patterns in the shoulders and upper back.
- Increased tension in the upper trapezius muscles (large muscle across the top of your shoulders/lower neck) and suboccipital muscles (muscles at the base of your skull), which can lead to jaw clenching and headaches.
- Altered tongue posture, affecting jaw alignment and breathing patterns.
This misalignment places excessive load on the TMJ and neck muscles, which can lead to pain, dysfunction, and reduced range of motion.
How Poor Jaw Posture Increases TMJ Muscle Tension
Poor jaw posture, such as letting the mouth hang open, clenching the teeth, or resting the tongue incorrectly can place excess strain on the muscles around the TMJ.
When the jaw isn’t in its natural resting position, muscles like the masseter, temporalis, and pterygoids (muscles that control the moth and jaw) have to work harder to support the joint. This leads to increased muscle tension, fatigue, and discomfort.
Over time, this overuse of the muscles can contribute to pain, jaw stiffness, and even headaches.
Additionally, as previously mentioned, poor posture in the neck and head (such as forward head posture) can further exacerbate TMJ dysfunction, creating a cycle of muscle imbalance and joint stress. Addressing jaw and neck alignment through targeted exercises and physiotherapy can help relieve this excess load and restore optimal function.
The Role of Deep Neck Flexors in TMJ Dysfunction
The deep neck flexors (DNFs), including the longus capitis and longus colli, play an important role in maintaining proper head and neck alignment,l and good jaw posture. These muscles help stabilise the cervical spine, particularly in the C2-C3 region, which is closely linked to TMJ function.
Weakness or dysfunction in the DNFs often leads to forward head posture, which shifts the jaw into a retracted position, as already discussed, this is a significant contributing factor for increasing strain on the TMJ and surrounding muscles.
Strengthening the deep neck flexors through targeted exercises helps restore proper head and neck positioning, reducing unnecessary load on the TMJ and improving overall jaw mechanics. This is why deep neck flexor training is an essential component of TMJ rehabilitation.
Lifestyle, Occupation, and Stress – daily Influences on TMJ Pain
Our everyday habits, work demands, and emotional stress levels can have a significant impact on TMJ function. People with high-stress lifestyles often unconsciously clench their jaw or grind their teeth (bruxism), particularly at night, which increases tension in the jaw muscles and overloads the TMJ.
Similarly, jobs that require prolonged sitting, especially at a desk or screen, can lead to poor posture, with forward head positioning and rounded shoulders; placing extra stress on the cervical spine and jaw structures.
Even habits like holding a phone between your shoulder and ear or chewing gum excessively can aggravate symptoms. Understanding and modifying these lifestyle factors can make a huge difference in managing TMJ pain.
At Complete Physio, we work closely with patients to identify contributing habits and stressors, and we integrate strategies such as ergonomic advice, stress reduction, and breathing techniques to support your recovery.
Assessment and Treatment at Complete Physio
At Complete Physio, we conduct a thorough subjective and objective assessment to understand the underlying cause of your jaw or neck pain. This includes assessing jaw movement, bite alignment, neck mobility, muscle tension, and posture.
We have a team of specialist physiotherapists who are highly experienced in treating TMJ problems. Things that they will be looking for include:
- Neck mobility restrictions – Limited movement or stiffness, particularly at C2-C3 level and into rotational neck movements.
- Tenderness and muscle tightness – In the suboccipital muscles (muscles at the base of your skull), which often become overactive in TMJ dysfunction.
- Postural imbalances – Forward head posture or asymmetries that contribute to jaw strain.
- Neural involvement – Assessing whether nerve irritation from the upper cervical spine is referring pain to the jaw.
Physiotherapy treatment may include:
- Relaxation techniques and lifestyle advice – To help reduce anxiety and stress which leads to clenching and grinding.
- Postural correction – Exercises to improve head and neck positioning, reducing strain on the TMJ.
- Manual therapy – Joint mobilisation techniques to restore movement at C2-C3.
- Soft tissue release – Targeting tight muscles in the neck and jaw.
- Neck and jaw coordination exercises – To improve muscle control and function.
- Muscle strengthening exercises – especially the deep neck flexors and scapular stabilisers.
- Mewing – This is a specific exercise working on your tongue and jaw position.
By addressing both the TMJ and cervical spine together, we provide a truly holistic approach to treating jaw pain, ensuring long-term relief and optimal function.
Injection Therapy for TMJ
If you have persistent, severe pain and symptoms that physiotherapy intervention alone is not alleviating, you may be a good candidate for injection therapy.
We work closely with our medical team to offer ultrasound-guided injections, led by Dr Matteo Bernardotto.
These include:
- Corticosteroid Injections – Corticosteroid works as a very effective anti-inflammatory treatment which will reduce pain in the TMJ.
- Botox Injections – These injections are used to relax overactive jaw muscles and relieve tension-related symptoms.
- Hyaluronic Acid Injections – These can help improve joint lubrication and function.
- PRP Injections – PRP is an injectable solution of a patient’s own blood platelets, which are rich in growth factors that promote healing and tissue regeneration – again helping to reduce pain and restore function.
Invisalign, Clear Braces, and Their Impact on TMJ Dysfunction
One other aspect of TMJ pain that is worth discussing, is how clear braces can also be a cause of TMJ problems.
Invisalign and other clear aligners have revolutionised orthodontics, offering a quick and discreet way to straighten your teeth.
However, while these devices can have a positive effect on the TMJ by improving bite alignment and reducing uneven pressure, they can also contribute to TMJ dysfunction in certain cases.
A thin mouthguard-like insert, such as Invisalign, can sometimes act similarly to a night guard, reducing teeth grinding (bruxism) and relieving joint strain. However, the process of tooth movement and prolonged wear of aligners can also alter jaw positioning, potentially increasing strain on the temporomandibular joint and surrounding muscles.
As the aligners gradually shift the teeth, they can change the occlusion (bite alignment), which may cause an imbalance in the way the jaw moves and functions. Some patients may unknowingly develop a habit of clenching or grinding their teeth against the plastic trays, again increasing tension in the jaw muscles.
This extra load on the jaw can lead to pain, clicking, restricted movement, and muscle fatigue – all common symptoms of TMJ dysfunction.
It’s incredibly important for your orthodontists to conduct a thorough TMJ assessment before prescribing clear braces. This should include an assessment of jaw movement, muscle tension, bite function, and any pre-existing TMJ dysfunction.
Without proper screening, patients with undiagnosed TMJ issues may find that their symptoms worsen as their teeth shift.
At Complete Physio, we frequently see patients who develop TMJ pain following orthodontic treatment, often due to inadequate assessment or lack of postural rehabilitation and muscle strengthening during the realignment process.
If you’re experiencing jaw discomfort during Invisalign/clear brace treatment, a collaborative approach between your orthodontist and one of our TMJ specialists can help ensure a healthy, pain-free transition to a better smile.
In Summary
TMJ dysfunction is rarely a standalone problem. The cervical spine and posture play a fundamental role in how the jaw moves and functions. By addressing the neck and jaw together, we can break the cycle of pain and improve overall function. If you’re dealing with persistent jaw discomfort, don’t just focus on the jaw – your neck may hold the key.
To book an appointment with one of our TMJ specialists at Complete Physio, give us a call or book online.
Don’t let pain hold you back, book now!