At Complete Physio, thumb CMC joint arthritis is one of the most common hand problems we see in our clinics, particularly in women.
Pain at the base of the thumb is something many women first notice in their late 40s or 50s. At first it may be subtle; a twinge when opening jars, aching after a day of cooking or gardening, discomfort when texting or scrolling on a phone.
Over time, it can become more persistent and frustrating.
This is not a coincidence; base of thumb arthritis (first CMC joint osteoarthritis) is significantly more common in women than men, particularly from mid-life onwards.
Understanding why this happens can help women recognise symptoms earlier, seek appropriate treatment, and avoid unnecessary fear about what lies ahead.
Key takeaways for women over 50
- Base of thumb arthritis is extremely common in women and often genetically influenced
- Symptoms frequently appear around mid-life
- Pain does not always mean rapid deterioration of function
- Physiotherapy, splints and injections are highly effective for many women
- Surgery is only needed in a minority of cases
The anatomy behind the problem
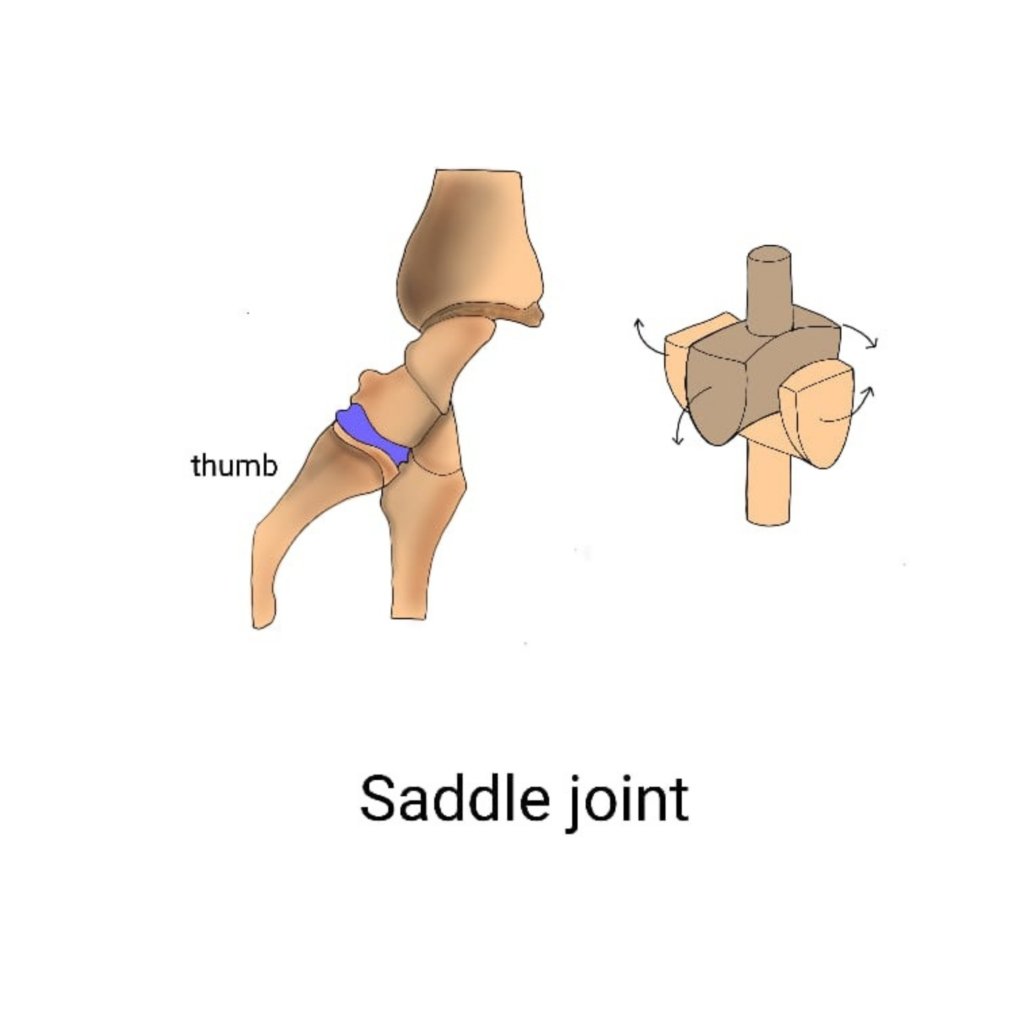
The base of the thumb is where the first metacarpal meets a small wrist bone called the trapezium.
This joint, the first carpometacarpal (CMC) joint, is known as a saddle joint which is what gives the thumb its extraordinary range of movement.
Unlike the fingers, which mainly bend and straighten, the thumb can:
- Pinch
- Twist
- Rotate
- Move across the palm
This mobility is essential for hand function, but it also makes the joint inherently less stable. The first CMC joint relies heavily on ligaments rather than bony shape for support.
Over time, those ligaments can stretch. When that happens, the joint loses its precise alignment (known as congruence), this then leads to abnormal joint loading and gradual wear and tear on the cartilage. This is the process that causes osteoarthritis of the CMC (base of thumb) joint.
Why women are more affected than men
Studies suggest that CMC OA is 3 – 4 times more common in women. There is no single reason for this, but several factors come together, which influence the condition.
1. Ligament laxity
Women, on average, have greater ligament flexibility than men. This is beneficial in many ways, but at the base of the thumb it can mean the joint is more prone to subtle instability over time.
Repeated pinching – gripping keys, jars, phones, kitchen utensils, gardening, cooking etc, gradually stretches the supporting ligaments. Eventually, the thumb metacarpal can begin to shift slightly out of position, accelerating cartilage wear.
2. Genetics
There is a strong hereditary element. Many women with thumb arthritis recognise the same changes in their mother’s or grandmother’s hands. You might notice a visible bump at the thumb base, a squarer-looking thumb, or difficulty with grip.
Genetics influence both joint shape and ligament quality, increasing vulnerability to the problem, long before symptoms appear.
3. Hormonal changes around mid and later life
Although research is still evolving, hormonal changes around menopause are thought to influence ligament strength and joint health. Reduced oestrogen levels may affect collagen quality, making ligaments less resilient to long-term load.
This helps explain the higher prevalence of symptomatic CMC OA after mid-life, even without a clear injury.
How the thumb is used
Thumb arthritis doesn’t develop from a single heavy activity, but from years of repetitive pinching and gripping movements during everyday tasks:
- Sports such as golf
- Food preparation
- Lifting and carrying
- Caring roles
- Phone and device use
- Using DIY tools
- Fine hand tasks at work
It is the accumulation of load, rather than extreme strain, that is the cause of the problem.
Common symptoms women notice
Women often describe symptoms as coming on gradually:
- Aching or sharp pain at the base of the thumb
- Pain with pinching or gripping
- Difficulty opening jars or bottles
- Reduced pinch strength
- Swelling or tenderness at the thumb base
- A visible lump or squaring at the base of the thumb
- Clicking or grinding sensations
Symptoms may flare for weeks or months, then settle again – which can be confusing and lead many women to delay seeking help.
Diagnosis: what actually confirms it?
In most cases, diagnosis is straightforward.
An experienced clinician can often identify base of thumb arthritis through:
- Careful examination of thumb position and movement
- Local tenderness and crepitus (grinding)
- Observation of subtle joint subluxation
Imaging
X-rays
X rays are used as the gold standard to confirm the diagnosis of OA, assess severity, and rule out involvement of neighbouring joints.
However, it is important to note that pain does not always match X-ray changes and treatment decisions are guided by symptoms and function, not just imaging alone.
Ultrasound imaging
X-rays show joint space narrowing, bone spurs (osteophytes) and alignment changes. However, X-rays don’t show the soft tissues that play a crucial role in this condition.
Increasingly, musculoskeletal ultrasound is recognised as a valuable alternative or complement to X-ray assessment, particularly in early or symptomatic cases.
Importantly, ultrasound findings often correlate more closely with pain and symptoms than X-ray changes alone.
In-clinic ultrasound at Complete Physio
At Complete Physio, we are able to offer diagnostic ultrasound as part of your initial assessment, performed by clinicians specially trained in musculoskeletal imaging.
For many patients, this means fewer delays, clearer answers, and a more personalised treatment plan, without needing referral for hospital-based imaging unless it is genuinely required.
MRI
MRI is not often used for diagnosing thumb OA.
Why many women fear “arthritis” more than they need to
A common concern we hear is:
“If this is arthritis, does that mean it will only get worse?”
The answer is not necessarily.
Base of thumb arthritis often behaves differently from hip or knee arthritis. Many women experience painful phases that settle over time, especially when the joint is supported properly and overload is reduced.
Importantly, the majority of women with base of thumb arthritis don’t need surgery.
Non-surgical treatment: what really helps
Specialist physiotherapy
Hand and upper limb physiotherapy is central to management.
Treatment focuses on:
- Improving thumb joint stability
- Strengthening key thumb and wrist muscles
- Optimising pinch technique
- Reducing joint strain during repetitive daily activities
- Strengthening wrist and forearm muscles to take some of the load off the smaller thumb joint.
This approach often provides significant pain relief and improved confidence in using the hand.
Splinting (used wisely)

Splints can be helpful, but are best used strategically:
- During painful flare-ups
- For specific activities that aggravate symptoms
Smaller functional splints such as a Push CMC brace, are the best options, as they support the joint without overly restricting hand use.
Injections for base of thumb (CMC) arthritis
While injections do not alter the underlying arthritis, they can be extremely valuable in settling painful flare-ups and creating a window in which physiotherapy, strengthening and activity modification can be progressed more comfortably.
The most commonly used option is a corticosteroid injection, which works by reducing inflammation within the joint.
Many patients experience meaningful pain relief, often within days, and this benefit can last for several weeks or months.
Other injectable options may be considered in selected cases, such as Hyaluronic acid and
Platelet-rich plasma (PRP), but current evidence remains limited, meaning they are not routinely recommended as first-line treatments.
At Complete Physio, injections are done under ultrasound-guidence, allowing accurate placement within the small CMC joint and improving both comfort and reliability.
Used appropriately, injections can delay or even avoid the need for surgery, while helping patients maintain hand function and quality of life.
What if symptoms persist?
When pain remains limiting despite conservative care, surgical options may be discussed. These include:
- Trapeziectomy (removal of the trapezium bone)
- Joint fusion in selected cases
- Thumb CMC joint replacement in carefully chosen patients
Modern joint replacement techniques have shown encouraging results in active women who wish to maintain strength and movement, although long-term data is still developing.
A specialist assessment helps determine which option, if any, is appropriate.
Struggling with thumb pain?
At Complete Physio, our specialist physiotherapists work closely with leading hand surgeons to provide clear diagnosis, personalised treatment plans, and evidence-based care.
Book an appointment with Complete Physio to get expert help for base of thumb arthritis.
References
- Srikanth, V.K., Fryer, J.L., Zhai, G., Winzenberg, T.M., Hosmer, D. and Jones, G., 2005. A meta-analysis of sex differences prevalence, incidence and severity of osteoarthritis. Osteoarthritis and cartilage, 13(9), pp.769-781.
- Wolf, J.M., Scher, D.L., Etchill, E.W., Scott, F., Williams, A.E., Delaronde, S. and King, K.B., 2014. Relationship of relaxin hormone and thumb carpometacarpal joint arthritis. Clinical Orthopaedics and Related Research®, 472(4), pp.1130-1137.
- Wolf, J.M., Turkiewicz, A., Atroshi, I. and Englund, M., 2014. Prevalence of doctor‐diagnosed thumb carpometacarpal joint osteoarthritis: an analysis of Swedish health care.
- Armstrong, A.L., Hunter, J.B. and Davis, T.R.C., 1994. The prevalence of degenerative arthritis of the base of the thumb in post-menopausal women. Journal of hand surgery, 19(3), pp.340-341.
Don’t let pain hold you back, book now!





