What is Plantar Fasciitis?
Plantar fasciitis is one of the most common conditions we see at Complete Physio and the number one cause of heel pain in the UK. It can also cause pain along the arch of your foot. Symptoms normally present gradually, often without any specific injury or trauma, and are regularly ignored by the sufferer for many months. It involves irritation and inflammation of the thick band of tissue, known as the plantar fascia, that runs across the bottom of your foot and connects the heel bone to the toes. It is a very important structure which provides stability and support to the entire foot.
Anatomy of the Plantar Fascia
The plantar fascia is a strong, fibrous band of tissue, that lies directly beneath the skin on the bottom of your foot. It connects from the heel bone (calcaneus) all the way to the big toe, and supports the entire foot, specifically the arches of your foot.

It also has an important role in normal foot biomechanics and helps to propel you forward during both walking and running. It is the most common structure in the foot to suffer injury and affects a large proportion of the population – it’s estimated 10% of people will experience this problem during their lifetime.
What are the causes of Plantar Fasciitis?
In most cases, plantar fasciitis develops without a specific, identifiable reason or injury. The plantar fascia is cleverly designed to absorb the stresses and strains that we place on our feet when walking, running, and doing other, normal daily and sporting activities. However, with overuse and/or as we get older, the fascia loses some of its elasticity and resilience, and the high force from activity can irritate or tear the plantar fascia. The body will always attempt to heal itself by initiating a natural inflammatory (healing) response. This inflammation is often what causes the heel pain and stiffness of plantar fasciitis. At first, the damage may only be minor and not cause any major problem, but if the injury progresses, it may become more painful and debilitating. Without the appropriate and timely rest and optimal treatment, inflammation of the plantar fascia will continue to be exacerbated, and the tissue may not be able to repair itself. This leads to a cycle of significant pain and dysfunction.
Risk Factors
While there is often no identifiable cause, there are, however, many factors that can make you more prone to developing this condition. This can be set out into 3 categories:
- Overloading or overuse of the fascia
- Spending many hours standing each day (postmen, teachers, policemen, nurses)
- Repetitive high impact activity (running, dancing, high impact sports)
- Starting an unaccustomed/new or a sudden increase of activity
- Wearing shoes with thin soles, or hard soled shoes, ballet pumps, or flip-flops
- Obesity
- Problems with the health of the Fascia
- Age – as we get older, tendons and ligaments tend to shorten and lose some flexibility, making the tissues stiffer and less able to tolerate stress (plantar fasciitis is most common among people aged 40 to 60)
- Diabetes – is a known risk factor of plantar fasciitis
- Biomechanical Factors
- Flat feet or high arches
- Tight calf muscles, or Achilles tendon
- Weak calf muscles and foot musculature
- An unusual walking or running gait
- Excessive weight/obesity
What are the symptoms of Plantar Fasciitis?
The main symptom of plantar fasciitis is heel pain, particularly when you first put your foot down in the morning or getting up after sitting for a period (known as ‘start up’ pain). The pain is often described as stabbing pain, throbbing, or a burning ache, that is typically exacerbated when the plantar fascia is used after a period of prolonged rest. Most people experience plantar fasciitis in one foot at a time, but it’s possible for it to affect both your feet at once. It can be a very painful, debilitating condition that causes significant distress and suffering.
The most common symptoms of plantar fasciitis include:
- Pain on the bottom of the foot near the heel
- Pain along the arch of the foot, sometimes accompanied by a ‘lump’ or thickening on the sole of the foot.
- Often exquisite, pinpoint pain on palpation.
- Pain when first getting out of bed, or after a long car ride. The pain often reduces or subsides after a few minutes of walking
- Increased pain with prolonged walking.
- Increased pain with exercise, especially higher impact activities. – Greater pain with the first 10 mins of activity, reduced pain during activity and then increased pain after exercise or activity.
If you are suffering from any of the above symptoms and would like to see one of our physiotherapists, please contact our clinic on 020 7482 3875 or email info@complete-physio.co.uk and someone will get back to you asap.
How do we diagnose Plantar Fasciitis?
It is very important for you to gain a speedy and accurate diagnosis of your heel pain, to make sure that you are treated timely and effectively. Please note, not all heel pain is plantar fasciitis and other conditions must be ruled out for example, in runners a common condition we do not want to miss is a calcaneal (heel bone) stress fracture.
At Complete Physio, our expert team of highly qualified clinicians will be able to accurately diagnose the cause of your heel pain during your initial assessment.
Clinical Assessment
At your first appointment your physiotherapist will begin by asking questions about your symptoms, what aggravates and eases your pain, your past health, and your normal daily routine and exercise regime. This will help to build up a picture of the probable diagnosis.
After the subjective consultation, your physiotherapist will complete a series of clinical tests to confirm their diagnosis; this may include:
- Gently, but skilfully, feeling around your heel and foot, to find exactly where it is most painful.
- Looking at your foot posture and assessing the range of movement of your foot and ankle.
- Testing the strength of your foot and lower leg muscles.
- Assessing muscle length and flexibility of calves, and Achilles tendon.
- Watching you move your foot and ankle, and how you perform activities such as walking, hopping, jumping and running.
- Checking other regions of the body, such as hips, knees, and lower back. This will help to identify if other areas are contributing to the problem.
These tests will confirm your diagnosis and help us understand why you have developed plantar fasciitis in the first place. Knowing the why as well as the what, enables your physio to provide the best and most appropriate treatment plan, tailored specifically to you, and will allow you to return to full function as soon as possible.
After your initial assessment, if your physio feels there might be an alternative diagnosis, or has any concerns regarding your symptoms, for example they suspect a tear in the plantar fascia, they may suggest that you have a diagnostic ultrasound scan. If a calcaneal stress fracture is suspected an X-ray or an MRI scan may be advised.
Diagnostic Ultrasound Scan
A diagnostic ultrasound image can be very useful to visualise the size and shape of the plantar fascia and to confirm the severity of the plantar fasciitis. It will also identify if you have sustained a tear in the plantar fascia or have a small nodule/lump on the plantar fascia, called a plantar ‘fibroma’. Identifying a tear or a ‘fibroma’ is important, as it will have an impact on your treatment. For example, certain treatment techniques such as a steroid injection or shockwave treatment may not be used if you have a tear and your physiotherapist may suggest a period of immobilisation in a walking boot if the tear is severe and/or occurred recently.
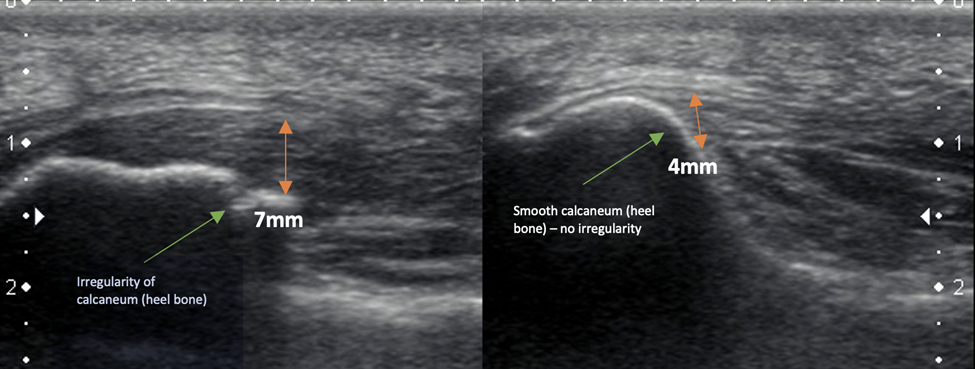
The ultrasound image on the painful left heel shows significant thickening and swelling of the plantar fascia and irregularity of the calcaneum (heel bone) in keeping with plantar fasciitis. No tear or fibroma is visualised. The ultrasound image on the right heel reveals the normal thickness and appearance of the plantar fascia on the painfree foot. Ultrasound allows for a direct side by side comparison, unlike an MRI scan.
At Complete Physio we can arrange for you to have an ultrasound scan at the clinic with one of our clinical specialists, who are dual trained physiotherapists and sonographers.
You do not require a GP referral for this scan.
If you already know that you need/want to have an ultrasound scan as part of your initial assessment, you will need to request this when you book your appointment, so that you can be booked in with an appropriate one of our clinical specialists.
Xray
X-rays provide clear images of bones and are useful in ruling out other causes of heel pain, such as fractures, stress fractures or arthritis. They do not show soft tissue and therefore have no role in the diagnosis of plantar fasciitis.
MRI
MRI scans are rarely required to diagnose plantar fasciitis. They may be used if the heel pain is not relieved by initial treatment methods or if your physio is concerned that a different problem is causing your heel pain.
How do we treat Plantar Fasciitis?
Physiotherapy Treatment
Once you have a diagnosis, your physiotherapist at Complete will firstly ensure that you have a clear understanding of your condition and answer any questions that you might have. They will also discuss your treatment goals with you, and together you will plan a tailored rehab programme that fits in with your needs and lifestyle.
This will often include:
- Relative Rest and modification of activity – considering the location of the injury, this can often be quite challenging. However, your physio will advise you on appropriate rest and activity modification to ensure that the pain settles, and the plantar fascia is able to heal.
- Pain Management – taping the foot to offload and reduce the pressure on the plantar fascia can help to reduce your pain. Ice can also be applied to the affected area.
- Pain medication such as paracetamol and/or anti-inflammatory, are often useful in the early stages of treatment; this should be discussed with a pharmacist or GP who can prescribe the most appropriate pain relief for you.
- Stretching Exercises – your physiotherapist may teach you self-stretching methods to improve muscle flexibility and help restore normal movement – especially for your calf muscles and Achilles tendon.
- Manual therapy – to help improve movement and reduce muscle stiffness, your physiotherapist may use manual therapy such as massage or soft tissue release techniques to the foot and calf.
- You can also carry out self-massage directly to the plantar fascia at home using a massage ball (a massage ball, golf ball or even a frozen water bottle will do the job!)

- Muscle strength – muscle imbalances and weakness in the muscles of your foot and lower limb can contribute to problems with plantar fasciitis. Your physiotherapist will design a resistance program to strengthen all your muscle groups, and ensure they are working together in synergy.
- Advise on footwear and orthotics – your physiotherapist will be able to offer you advice on the best type of footwear for you, and if required, they can fit you with some insoles for your shoes. If they feel further assessment is required then they may refer you for a full podiatry gait analysis, with one of our highly specialised podiatrists.
- Biomechanical and movement re-education – this may involve teaching you how to correctly squat, lunge, run or jump.
- Functional and sports specific training – once your pain, strength, and range of movement improve, functional training can help you safely resume more demanding activities and get you back to the exercise/sport that you enjoy.
What can I do if physiotherapy treatment is not helping?
Physiotherapy will always be the key component of treatment for plantar fasciitis, however if your symptoms are not responding to initial treatment, we have other options at Complete Physio that can be used to improve your pain and help the plantar fascia to heal.
Shockwave Therapy – also known as Extracorporeal Shockwave Therapy (ESWT) for patella tendinopathy
Shockwave therapy can be used alongside your rehabilitation programme to help significantly reduce your pain and speed up your recovery.

Shockwave is an effective, evidence-based treatment option for treating plantar fasciitis. It produces a series of powerful sound waves which provide a small dose of controlled microtrauma to the fascia. This has shown to stimulate the body’s natural healing process, initiating new tissue healing. It also desensitises irritated nerve endings that surround the painful tissue, resulting in pain and symptom reduction.
Recent evidence suggests positive outcomes following 3-5 shockwave treatment sessions.
We are able to offer ESWT at three of our clinics – Bury Street (next to Gherkin), Chelsea and Angel clinics.
Ultrasound-Guided Injection
If your pain is persistent and nothing else is working to resolve your symptoms, then injection therapy may be required. Injection therapy is used within musculoskeletal medicine to reduce pain and inflammation, allowing you to resume your physiotherapy.
There are two ultrasound guided injection options for plantar fasciitis: cortisone or platelet rich plasma (PRP) injections:
- Ultrasound guided steroid injections (also known as cortisone or corticosteroid injections) involve a mixture of local anaesthetic and corticosteroid (a potent anti-inflammatory) being injected around the plantar fascia, under the guidance of a real-time ultrasound scan. This normally provides rapid pain relief within a few days allowing to walk with less pain. Using ultrasound guidance ensures the plantar fascia is accurately targeted. Research has shown that guided injections are more accurate and are more effective at reducing pain than non-guided injections. Normally only one injection is required. For more information about steroid injections see our FAQ’s.
- Platelet rich plasma (PRP) injections are a drug-free, natural injection option which can provide long lasting pain relief. The injection is carried out under ultrasound guidance and may be recommended if a tear is identified on diagnostic ultrasound. The research suggests between 1-3 injections be carried out, depending on the severity of your condition, how long you have had the problem and how you respond to the treatment. The injection involves our clinician taking blood from your arm (just like a blood test), spinning your blood in a centrifuge for 5 minutes to produce the PRP. This is then injected around and into the plantar fascia using ultrasound guidance. PRP encourages and stimulates a new healing response in the plantar fascia to help improve the structure and strength of your plantar fascia.
Complete Physio offers a unique injection service and has a dedicated team of highly experienced physiotherapists and musculoskeletal sonographers. All of whom are fully qualified to prescribe medication, scan and inject. For further information, please contact us on 0207 482 3875 or email injections@complete-physio.co.uk.
Surgery For Plantar Fasciitis
It is extremely rare that surgery is required for heel pain, however if none of these treatments are effective, and you have unresolved pain that is significantly affecting your normal daily life, you may be referred to an orthopaedic specialist for a surgical review.
A surgical referral should only be considered if all other treatment options have been exhausted.
There are two main options for surgery:
- Gastrocnemius release lengthens the calf muscles to increase the range of movement in the ankle, reducing stress on the plantar fascia. The surgeon will often use a minimally invasive technique, which may reduce recovery time.
- Plantar fascia release involves making a small, precise cut in the plantar fascia to reduce tension. People with a good range of movement in the ankle are better candidates for this procedure.
If you are suffering from heel pain and would like to see one of our physiotherapists, or to find out what we can do to help you, please contact our clinic on 020 7482 3875 or email info@complete-physio.co.uk
Don’t let pain hold you back, book now!