This condition is also known as Achilles tendinitis, enthesopathy and insertional calcific tendinopathy (although these are slightly different conditions these terms often get used inter-changeably)
1. What is insertional Achilles tendinopathy?
Insertional Achilles tendinopathy is a common cause of posterior heel pain in both sedentary and active people. It is often a chronic, frustrating injury which effects active adults aged between 30 and 60 years of age, particularly those who are engaged in regular sporting activity such as running (Zhang et al., 2020; Furia, 2006).
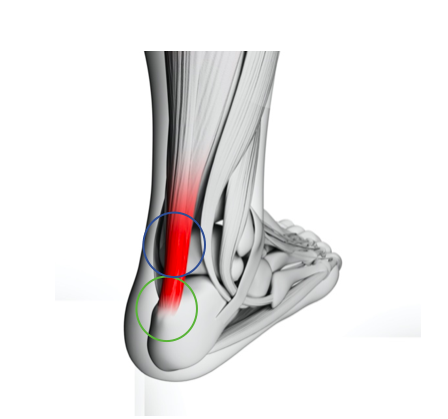
It is characterised by pain, swelling, morning stiffness and tenderness on the attachment of the Achilles tendon onto the heel bone, known as the calcaneum (green circle on the image below).
The other common type of Achilles tendon injury is called mid-portion Achilles tendinopathy. This injury is located above the heel bone towards the muscle belly (blue circle on the image below). Both mid-portion and insertional Achilles tendinopathy can be a very painful and debilitating condition which can be difficult to treat.
2. What causes insertional tendinopathy?
Insertional Achilles tendinopathy is associated with injury and/or overuse. However, while the exact cause is often unknown, there are certain risk factors such as impact based sports and activities such as running, tennis, volleyball and football. This condition is particularly common in runners who have:
- increased their mileage too quickly
- started running too often
- recently incorporated hill training
- changed their running shoes
Some individuals are genetically prone to tendon issues particularly those with collagen (connective) tissue conditions. Those who are overweight, diabetic or have high cholesterol are also more likely to get insertional Achilles tendinopathy and often these patients take longer to fully recover. Advancing age has also been shown to be a known risk factor.
Other intrinsic risk factors include hyperpronation (flat feet), stiffness in the ankle joint or hips and/or a leg length discrepancy (Furia, 2006).
3. How do we treat Achilles tendinopathy?
Most Achilles issues resolve with a course of physiotherapy. It is not unusual for this to take 6-12 weeks if the condition is chronic i.e. if you have had it longer than 12 weeks. Research shows that treatment should involve heavy slow resistance training for the calf muscle and Achilles tendon.
If you are not improving with rehabilitation and physiotherapy, shockwave therapy or an ultrasound guided injection may be an appropriate adjunct to your treatment.
At Complete we advise the least invasive treatment first. Shockwave is a non-invasive approach to the management of insertional Achilles pain. Ultrasound guided injections do have a role for some Achilles complaints but are generally reserved for the difficult cases that have failed physiotherapy and shockwave therapy.

3. Is shockwave therapy effective for insertional Achilles tendinopathy?
The quick answer is yes. It has been shown that shockwave is an effective option for treating chronic insertional Achilles tendinopathy, particularly when other nonoperative treatments have failed such as physiotherapy, rest, orthotics and medication (NSAIDs) (Al-Abbad and Simon, 2013, Mani-Babu et al., 2015).
At Complete we treat hundreds of clients every year with insertional Achilles tendinopathy and the combination of shockwave therapy and rehabilitation exercises has improved our clinical outcomes.
The use of shockwave therapy for Achilles tendinopathy is well supported by the National Institute for Health and Care Excellence (NICE). NICE provides national guidance and advice to improve health and social care. It provides evidence based recommendations to guide best practice within healthcare.

A systematic review and meta-analysis demonstrated that shockwave therapy for insertional Achilles tendinopathy is an effective treatment modality (Al-Abbad and Simon, 2013). A randomised controlled trial (RCT) of 50 patients (Rompe et al., 2008) compared shockwave with eccentric exercises. The study found statistically significant improvement for outcomes of pain and function at 4-month follow-up in the shockwave group.
A large case-control study (Furia, 2006) consisting of 68 patients compared shockwave with conservative treatment including rest, footwear modification, anti-inflammatory medication, gastrocnemius-soleus stretching and strengthening (n=34). The study demonstrated shockwave was statistically significantly better in improving pain. In fact, an average pain reduction of 5 on a 10 point visual analogue scale (VAS) was experienced by the patients i.e. this is a minimum of 50% pain reduction.
It is concluded that shockwave therapy is more effective than physiotherapy and rehabilitation alone for insertional Achilles tendinopathy. In one study, the more sports-active patients had better clinical outcomes than non sports-active patients after 5 years of follow-up (Zhang et al., 2020). This study also showed that following a course of shockwave therapy the symptoms continue to improve for several years afterwards. Furthermore, there was a very low reoccurrence rate in the shockwave group. This is particularly important because Achilles problems have a high reoccurrence rate.
Another study found that shockwave resulted in a greater decrease in pain on a 10 point scale than a traditional eccentric exercise program at 6-month and 18-month follow-up (Wei et al, 2017).
Scientific evidence clearly exists to support the role of shockwave therapy in insertional Achilles tendinopathy. At Complete we believe the combination of shockwave and rehabilitation provides the best treatment option for this condition.
4. How many sessions and how often do you need shockwave therapy for insertional Achilles tendinopathy?
At Complete we follow the latest evidence based recommendations for our shockwave protocols (see below). A minimum of three shockwave sessions approximately one week apart is recommended. Some patients require more than three sessions, but this will depend on how you respond to your initial treatment.
Recommendation: Deliver 2000 impulses at 2.5 bars (energy flux density 0.12 mJ/mm2) at 8Hz for three sessions at weekly intervals (Korakakis et al, 2017).
5.How long does it take to recover from insertional Achilles tendinopathy?
This does vary from person to person depending on the exact nature and extent of the injury. It is not unusual to feel an immediate reduction in pain following your first shockwave session. The likely scenario is a gradual reduction in pain over the following weeks to months.
6. Should you have an ultrasound scan before having shockwave therapy?
It is not always necessary to have an ultrasound scan before embarking on a course of shockwave therapy. Your physiotherapist will carry out a full assessment of your tendon and surrounding structures and ascertain if you require a scan before commencing shockwave therapy.
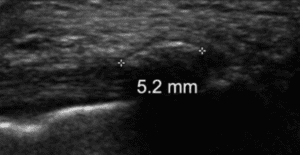
An ultrasound scan can be useful to further assess your tendon and confirm your exact diagnosis. An ultrasound scan (see image below) is better than an MRI scan for assessing the insertion of the Achilles tendon (Zhang et al., 2020). At Complete we carry out an ultrasound scan at no extra charge and you do not require a GP referral. If you would like a diagnostic ultrasound scan, please ensure you inform the reception team when making a booking.

An ultrasound scan will answer the following questions:
-
- Do you have a bursitis? – a bursa is a thin fluid filled sac which can become inflamed. An inflamed bursa is called a bursitis. There are two types of bursitis related to insertional Achilles tendinopathy: 1/ retrocalcaneal bursitis, or 2/ pre-Achilles/subcutaneous Achilles bursitis
-
- Is there calcification (bone) within your tendon? – this is known as ‘calcific tendinopathy’ or on occasion is called a bony spur.
-
- Is there a tear in your tendon? – if there is a tear, how large is the tear i.e. what grade tear is it?
-
- What is the severity of your tendinopathy? – is it mild, moderate or severe?
If you would like to book an appointment or would like more information before booking please call 020 7482 3875 or email info@complete-physio.co.uk
References:
Rompe, J.D., Furia, J. and Maffulli, N., 2008. Eccentric loading compared with shock wave treatment for chronic insertional achilles tendinopathy: a randomized, controlled trial. JBJS, 90(1), pp.52-61.
Wei, M., Liu, Y., Li, Z. and Wang, Z., 2017. Comparison of clinical efficacy among endoscopy-assisted radio-frequency ablation, extracorporeal shockwaves, and eccentric exercises in treatment of insertional Achilles Tendinosis. Journal of the American Podiatric Medical Association, 107(1), pp.11-16.
Zhang, S., Li, H., Yao, W., Hua, Y. and Li, Y., 2020. Therapeutic Response of Extracorporeal Shock Wave Therapy for Insertional Achilles Tendinopathy Between Sports-Active and Nonsports-Active Patients With 5-Year Follow-up. Orthopaedic Journal of Sports
Don’t let pain hold you back, book now!