1. What is Mid-portion Achilles tendinopathy?
Mid portion Achilles tendinopathy is a common overuse soft tissue injury with incidence rates reported to be between 1.85- 2.16 per 1000 people in the general population (de Jonge et al., 2011, Albers et al., 2016).
Achilles tendinopathy is common in running populations, with prevalence rates up to 9.5% (Lopes et al., 2012). Additionally, mid-portion Achilles tendinopathy affects inactive populations with 1 in 3 people with the condition leading a sedentary lifestyle (de Jonge et al., 2011).
Increased age and obesity are contributing factors for the condition as it is reported most frequently by people aged between 40 and 59 years (Yasui et al., 2017) (de Jonge et al., 2011).
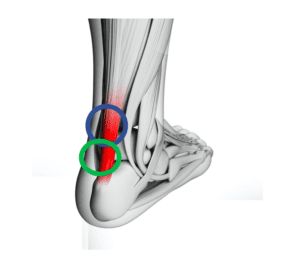
Mid portion Achilles tendinopathy is characterised by pain in the middle of the tendon, which is 2-6cm higher (see blue circle) than the heel bone (calcaneum) (Rompe et al., 2009, Furia, 2008). Patients also present with swelling and report morning stiffness of the tendon (Cook & Purdam., 2009).
Another common type of Achilles injury is called insertional Achilles tendinopathy, and this also appears as pain, swelling, morning stiffness but the tenderness is lower, at the attachment of the Achilles onto the calcaneum (see green circle).
2. What causes mid portion Achilles tendinopathy?
mid portion Achilles tendinopathy is associated with injury and/or overuse.
The precise cause is often unknown, but there are certain factors and sports such as running, tennis and football which can provoke the condition. Mid portion Achilles tendinopathy is particularly common in runners who have:
- increased their mileage too quickly
- are running too frequently
- very old and/or new running shoes
- have reduced ankle range of motion
- have reduced calf strength (Van Der Vlist et al., 2019)
3. How do we treat Achilles tendinopathy?
Most Achilles tendon issues resolve with a course of physiotherapy. It is however common for Mid portion Achilles tendinopathy to take 6-12 weeks if the condition is chronic (if you have had it greater than 12 weeks). Research shows that treatment should involve heavy loading/strengthening for the calf muscle and Achilles tendon.
If you are not improving with rehabilitation and physiotherapy, shockwave therapy or an ultrasound guided injection may be an appropriate adjunct to your treatment.
Shockwave is a safe, well-tolerated and non-invasive approach to the management of Achilles tendinopathy (Stania et al., 2019)
Ultrasound guided injections are generally utilised for the problematic cases that have failed physiotherapy and shockwave therapy.

4. Is shockwave therapy effective for mid portion Achilles tendinopathy?
Yes, shockwave is a very effective treatment modality for the treatment of mid portion Achilles tendinopathy.
Furia (2008) reported 34 patients with mid portion Achilles pain were treated with a Shock-wave therapy and 34 patients with were treated with another type of therapy (control group). After the treatment, the shockwave group had a statistically significant pain reduction and reported an excellent or good recovery.
A randomised controlled trial of 75 patient split into three different groups:
a) Tendon loading
b) Shockwave therapy and
c) wait and see, demonstrated positive results.
The tendon loading and shockwave therapy groups had improved function and less pain. 60% of the tendon loading and 52% of the shockwave therapy groups testified they were “completely recovered” or “much improved” (Rompe et al., 2009). At Complete we use a combination of both the tendon loading and shockwave therapy to get our clients out of pain and back to full function.
We believe it is the combination of therapies that is the key to our success.
These conclusions were reinforced and developed in a study of 68 patients, which involved combining the tendon loading and shockwave therapy, and the results demonstrated an increase in the proportion of “completely recovered” or “much improved” patients to 82% (Rompe et al., 2009).
Finally, Santamato et al ‘s (2019) results revealed a significant pain reduction in patients with mid portion Achilles tendinopathy along with improvements in ankle range of movement both short and long term. Furthermore, there was improved functionality and a positive clinical impression with patients reporting an excellent/good clinical picture.
At Complete we treat a large number of clients every year with mid portion Achilles tendinopathy and the combination of shockwave therapy and rehabilitation exercises has improved our clinical outcomes.
The use of shockwave therapy for Achilles tendinopathy is well supported by the National Institute for Health and Care Excellence (NICE). NICE provides evidence based recommendations to guide best practice within healthcare.

Scientific evidence undoubtedly supports the role of shockwave therapy in mid portion Achilles tendinopathy. The combination of shockwave and rehabilitation/tendon loading provides the best treatment outcome for this condition.

5. How many sessions and how often do you need shockwave therapy for mid portion Achilles tendinopathy?
At Complete we are guided by the latest evidence-based research for our shockwave protocols (see below). A minimum of three shockwave sessions roughly one week apart is recommended. Some patients require additional sessions, but this will depend on how you respond to treatment.
Recommendation: Deliver 2000 impulses at 3.0 bars (energy flux density 0.1mJ/mm2) at 8Hz for three sessions at weekly intervals (Korakakis et al, 2017).
6. How long does it take to recover from mid portion Achilles tendinopathy?
This varies from individual to individual depending on the type and severity of the tendinopathy. Some patients feel an instant decrease in their pain following the first shockwave session.
7. Should you have an ultrasound scan before having shockwave therapy?
The use of an ultrasound scan can be valuable to further assess your tendon and confirm your particular diagnosis. An ultrasound scan is superior than an MRI scan for assessing the mid portion of the Achilles tendon.
At Complete we undertake an ultrasound scan at no extra cost, and you do not need a GP referral. If you require a diagnostic ultrasound scan, please inform the reception team when booking. An ultrasound scan will assess if there is a tear in your tendon and/or tendinopathy. It will also identify is there is associated bursitis surrounding the Achilles tendon.
If you would like to book an appointment or would like more information before booking, please call 020 7482 3875 or email info@complete-physio.co.uk
References:
Don’t let pain hold you back, book now!





Leave A Comment