Why does my back hurt?
Back pain affects a significant percentage of the UK population every year. It is one of the most common reasons for people taking sick leave from work, and it costs the economy billions of pounds.
There are lots of different types of pain; often people experience back pain after sitting at work all day, or suffer from a burning pain in the hamstrings when driving, or feel as stiff as a board when getting out of bed in the morning.
If you’re wondering why your back is hurting, you’re not alone; 1 in 6 adults in the UK currently have back pain!
In this blog we will discuss the following:
- The difference between back pain and sciatica.
- Anatomy of the spine.
- What causes back pain and sciatica.
- What the common symptoms are.
- Who is likely to suffer from these conditions.
- Diagnosis and scans.
- The role of exercise and Physiotherapy.
What’s the difference between back pain and sciatica?
There’s lots of terminology surrounding back symptoms. Let’s first look at sciatica.
What is sciatica?
Sciatica is a general term which has come to mean pain that radiates along the sciatic nerve. In the clinical world we use the term ‘radiculopathy’, which means compression or irritation of a spinal nerve. The sciatic nerve is a very big nerve formed from the five lumbar nerve roots which are in the lower spine. It runs through the buttock and hamstring area and down into the foot.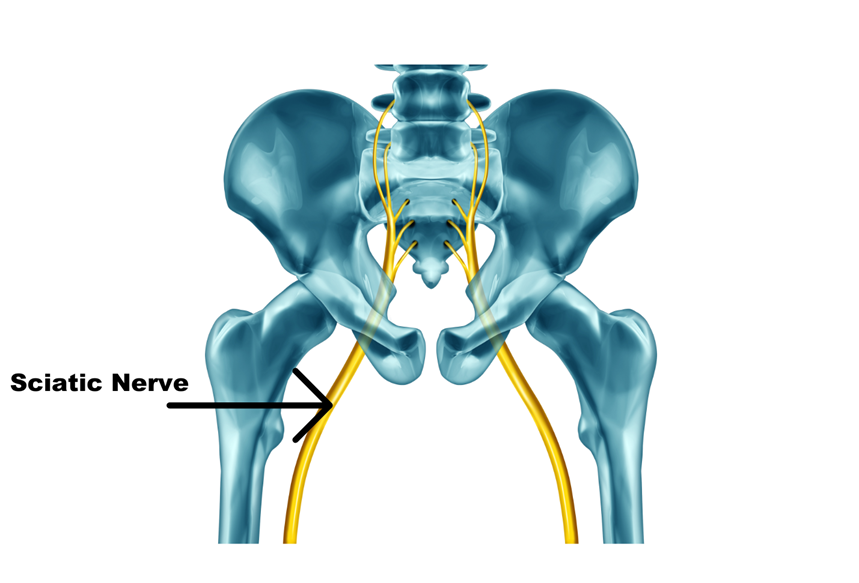
Who gets sciatica?
In the UK, it’s thought that each year, around 2.2% of people experience sciatica (Koes et al, 2007) and it tends to be more common in middle aged men.
We know from twin studies (Livshits et al, 2011), that some people have a predisposition to sciatica, but being overweight (Samartzis et al, 2014); being a smoker; or having diabetes can also increase your risk.
Interestingly, when it comes to physical work and the prevalence of sciatica, it’s less about how much weight you carry, rather, it’s more about how used to it you are. If you have a very sedentary job and you occasionally have to pick up heavy loads, you have a higher risk of developing sciatica than someone who carries heavy loads all the time, and in fact, research suggests heavy load carrying may even be protective (Euro et al., 2019). This is similar for someone who has been away from the gym for a long period of time and then returns and tries to go back to previous levels of activity or weights, but gets back pain. This is because they are no longer accustomed or conditioned to such activity or loads. A progressive return to the gym and lifting is always recommended.
“I had my first ‘episode’ of a bad back when I left university, and I started to work long hours in consultancy. I’d sit for 12 hours a day, five days a week, and only have time for sport at the weekends. I started an online high intensity training class during lockdown, overdid it a bit, and I began to have a nagging ache in the bottom of my back. Pretty soon it hurt just even bending over to clean my teeth, and I found sitting unbearable”
(Sarah, 25, London – Complete Physio patient)
What are the symptoms of sciatica?
Although the sciatic nerve originates from the low back, not everyone who has sciatica experiences back pain; it is often more common to have pain in the leg. Some people will experience tingling (aka pins and needles), numbness, or a burning sensation, for others, it might feel like a deep ache in their buttock or the side of their calf. It’s usually felt in one leg, but it is possible to have sciatica affecting both legs.
Sciatica pain can come and go, but many people will find sitting or driving to be painful, and they may feel the need to stand up, or walk around when the pain comes on. Straining when coughing or going to the toilet can worsen the pain and frustratingly, the pain can sometimes disturb your sleep.
Occasionally, weakness can occur because of a spinal nerve being compressed, which might show up as loss of power in the leg, or foot drop. A serious, but very rare consequence of nerve compression is cauda equina. This can lead to loss of bladder and bowel control, as well as severe leg weakness (often in both legs), and it’s a medical emergency – if you think you have this, you must see a doctor urgently.
Thankfully, the majority of people who experience sciatica have fairly mild symptoms, and make a significant recovery within a few weeks, although it can take longer to fully resolve.
“In 2018 I began to experience dreadful back pain and sciatica symptoms. My private health insurance had a pathway that linked me with a physio, who made a diagnosis over the phone. Unfortunately, it was the wrong diagnosis, and my first experience of physio was a bad one. My symptoms worsened and I saw two further physios; one of them left me with worse pain, and the other helped me, but only temporarily.
Out of desperation I saw a Consultant Spinal Surgeon, and I was diagnosed with three prolapsed discs. I eventually agreed to undergo some injection treatment. The consultant told me that I really need to pick up again with physio, because my core was very deconditioned (I’m a sedentary middle-aged woman who has never and will never be sporty!).
I was very sceptical that any further physio could help me, but the Consultant reassured me that the clinic he was sending me to offer expert assessment and treatment for spine problems. The care and treatment I received has made all the difference in the world, and I am now pain free. I also have a much better understanding of how I can prevent further episodes and am doing my best to keep up with my exercises in the long term”
(Stephanie, 56, Hertfordshire – Complete Physio patient)
What causes sciatica?
Disc Herniation
One of the most common reasons a nerve root becomes compressed is because of a bulging, herniated, or ‘slipped’ disc. Discs are the ‘cushions’ that sit between the vertebrae bones of the spine. The lumbar discs are made of a tough, fibrous outer ring, known as the ‘annulus’, and the centre of the disc (the ‘nucleus pulposus’) is more jelly-like. Sometimes there may be tearing of the annulus and the central disc material is released, irritating a nerve root.
Facet Joint Irritation
Sometimes a natural wear and tear process within the discs causes them to lose height which is often combined with wear and tear in the small joints at the back of the spine called facet joints. This can lead to narrowing of the foramina (holes) where the spinal nerve roots exit the spine, causing nerve irritation, or it can also narrow the central channel where the spinal cord sits. This is known as spinal stenosis, and can also cause symptoms of sciatica.
Slipped Vertebrae
Spondylolisthesis is the process of an abnormal slippage of one vertebrae on another, and it may occur because of small malformations in the spine (called pars defects), or because of wear of the facet joints. This may occasionally lead to traction or compression of the nerve roots.
And finally, there are rarer causes of sciatica, such as major trauma, and tumours. Thankfully, we don’t see these often, but if you’re experiencing pain that’s not shifting, it is an indication to see a clinician about your symptoms sooner, rather than later.
How is sciatica diagnosed?
Sciatica is a clinical diagnosis. If you have a history of sciatica symptoms, and if on examination your pain is provoked by a straight leg raising, or the ‘slump’ test, you likely have sciatica.
Do I need an MRI scan if I have sciatica?
Most people with sciatica symptoms won’t need an MRI; they need to get on with physio treatment, and their symptoms will usually settle.
It’s important to understand that our lumbar spine goes through a normal ageing process over time – it’s a bit like getting grey hair. If we carry out an MRI scan on a person who has no pain or symptoms, we’ll often see age-related changes, such as disc bulges or facet joint wear. Additionally, some people with back pain may have a very normal looking MRI.
Occasionally MRI scanning can be needed if a person has really severe pain that’s not improving or is worsening, if a person has concerning medical history, such as cancer, or if a decision needs to be made about additional other treatments (such as injection treatments).
Not all pain felt in the buttock or the leg is sciatica.
If you’ve got pain in your leg that’s showing up every day, it’s a really good idea to get a proper assessment from a physiotherapist (rather than relying on Dr Google!). Sometimes your problem isn’t sciatica; it may be hamstring tendinopathy, pain referred from the facet or sacroiliac joints, or even a vascular problem.
Not all back pain is sciatica.
When we consider the statistics, sciatica isn’t that common; most people presenting with back pain have, well, back pain! Back pain affects around a third of the UK’s adult population each year, with 1 in 15 people seeking help from their GP (Savigny et al., 2009).
What is back pain?
Back pain is felt in the back (obviously) and unlike sciatica, it doesn’t refer down the leg. Most back pain isn’t a sign that something bad is going on, and there isn’t usually a single cause or structure that’s the issue; it is often diagnosed as non-specific back pain.
Some people can feel anxious about the meaning of their pain, or feel afraid to move if they have pain. We know that movement is helpful, not harmful in this scenario, and helping people to understand that pain doesn’t equate to ‘damage’ is a big part of how we as physios can help people. The problem can be compounded by investigations and language used by the medical community. Radiological terms like ‘degenerative disc disease’ can be unhelpful, when often these are simply age-related changes, and nothing to fear. Our backs are strong, they are meant to bend, and they are built for lifting.
At Complete Physio we regularly meet people who are doing a lot of exercise or gym work, but all too often their choice of exercise isn’t serving them well, and their technique is poorly executed, resulting in them developing pain.
Additionally, some people are so overwhelmed with work, that they feel they can’t prioritise exercise in their daily routine. So, when they sit for 12 hours a day in an office chair it’s no surprise that prolonged, static postures bring on their back pain.
At the extreme end of the spectrum are athletes. I frequently work with dancers and people in the performing arts world, and many of them shut out their pain, believing that the pain will just go away. That strategy may work for a while (dancers are very tough cookies!), but eventually they may be unable to jump or perform a particular choreographic routine when their body finally declares ‘enough is enough!’
Does poor posture cause back pain?
In truth, there is very little research evidence to support the concept of poor posture (e.g. slouching) causing back pain, or the correction of poor posture preventing, or ‘fixing’ back pain. Instead, it may be more helpful to think of how we ‘tax’ our bodies with our daily choices. Sitting per say isn’t injurious, but hours of continuous sitting at an ill-set up workspace can bring on discomfort. Most low-back pain is what’s known as nonspecific. It’s not possible to identify a single origin of the pain. The good news is, we know what helps, and that is activity!
Exercise and back pain
When some people experience back pain (or sciatica), their response is to freeze, not want to move, and to rest in bed; often because the pain may seem alarming to them, and they may feel they are doing the right thing by resting their back. In almost all situations this is an unhelpful thing to do, because people recover faster without bedrest, and long periods of lying down weakens muscles and exacerbates stiffness.
Movement, on the other hand, is good for looking after our backs. Walking is actually one of the best exercises for back pain; A brisk 10-minute walk each day has lots of health benefits and counts towards your 150 minutes of weekly, moderate exercise, as recommended in the government’s physical activity guidelines for adults aged 19 to 64.
There are so many different ways to exercise these days, from sports, gym classes, virtual home based videos and Apps, to personal trainers and performance coaches; the variety and range of activities is endless. The most beneficial tends to be doing something that you enjoy and want to maintain in the long term.
At Complete Physio we believe in going back to basics when it comes to exercise to help back pain, and enabling people to perform everyday movements well, and in a way that suits their natural biomechanics and personal goals.
If there is something specific that you are having difficulty with, or that you want to work on, then your therapist will be able to assess that in more detail and tailor your rehab programme accordingly.
For example, if someone’s goal is that they want to deadlift comfortably, we will break down that movement into its component parts. Initially introducing a few warm up exercises to mobilise the lumbar spine, before focusing on posterior chain strengthening such as reverse lunges and bridges (Tatryn et al., 2021). We’ll then start to piece together the individual movement phases that make up a deadlift (lift off, pull through and lock out), initially using an unweighted bar before slowly progressing and adding weight. (In case you’re wondering if deadlifting is bad for your back, it’s not! – if done correctly; and in fact regularly carrying heavy loads has shown to be protective against back pain (Euro et al., 2019)).
If people have pain doing their chosen sport or activity, it is really important to find ways for them to tweak how they’re training, or find an alternative activity, rather than have them stop exercising completely. At Complete we understand that for many people exercise is their passion and helps with not only physical health, but mental health. It might be that for a short period of time good old-fashioned walking is all that you can manage, but we will always offer you support to continue to keep up a level of activity, and give you choices with exercise. We ensure that all our patients are treated as individuals and know how important it is to build trust and rapport with someone in order to get the best results.
“From the moment I met Genevieve at Complete Physio, I knew that she totally ‘got’ me. She knew I never wanted to run or be super active, but I did want to get out of pain. She was totally accommodating in her approach to my rehab – she gave me simple exercises that I could actually fit into my day. For the first time ever, I can say I have a ‘core’ – I’ve never had a core before!
The difference the therapy has made has been enormous; it’s transformed me.
Every morning I do my 10 minutes of rehab, and sometimes I’ll repeat it in the evening if I’ve been glued to my work desk all day.Genevieve gave me a rehab routine that I will actually do, and I feel the direct benefits from it. If you’re sceptical about physios, see Gen; she listened to my concerns and made me feel relaxed and confident.”
Rachel Rowan, Back pain sufferer
If you are experiencing any symptoms of back pain or sciatica, it is vital that you see a professional early, in order to get an accurate diagnosis and start an appropriate treatment plan. At Complete we have a highly experienced team of specialists who can help. Book an appointment through our admin team today by calling 020 7482 3875 or email us at info@complete-physio.co.uk
References:
Don’t let pain hold you back, book now!






