
What is degenerative disc disease (DDD)?
Degenerative disc disease is one of the most common causes of low back and neck pain. It generally affects the lumbar and cervical spine; it can also occur in the thoracic spine but this is far less common.
The term degenerative disc disease is rather misleading, as it is not actually a disease, but rather a normal process of ageing. After the age of 40, most people have some “wear and tear” i.e. degeneration, on their spinal discs, this is considered normal age related changes. Most of the time it occurs without pain and you do not even know about it!
As we get older, the thick spongy discs that cushion the vertebrae (the individual bones in your spine) and help to stabilise the spine begin to dry out and gradually deteriorate.
The purpose of this article is to help you better understand:
- The anatomy of the spine and the discs relating to degenerative disc disease
- The causes and symptoms of lumbar and cervical degenerative disc disease
- How degenerative disc disease is diagnosed
- The treatments that are available to you to help manage this condition and allow you to lead a full and active lifestyle.
Anatomy of the Spine and Spinal Discs
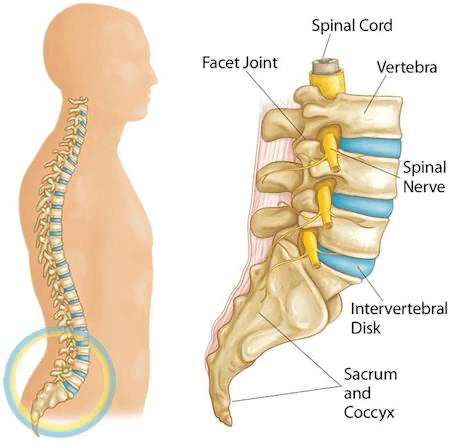
Your spine is made up of a long vertical column of moveable bones called vertebrae. These vertebrae are grouped into divisions called the cervical (neck), thoracic (upper back), and lumbar (lower back). There are 33 vertebrae in total and between each vertebra is a shock-absorbing disc that prevents the bones from rubbing together.
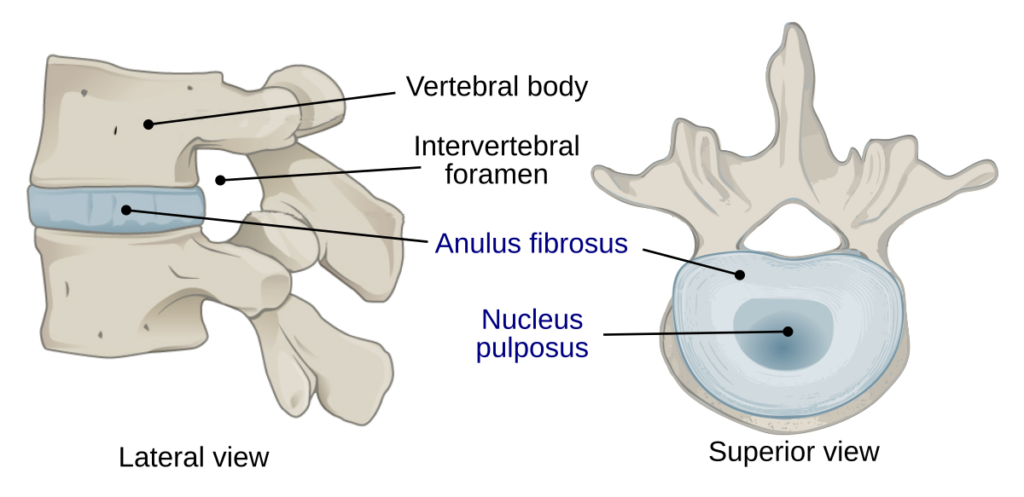
Discs are designed a bit like a tire (see images below); the tough outer wall (annulus), is made up of dense fibrous bands that attach to each vertebra bone. It also provides stability to the disc, and helps control the amount the disc moves. Inside the disc is a gel-filled centre called the nucleus, which changes shape to adapt to different loads – much like the inner tube.
It is very important that there is enough space between each vertebrae, to ensure normal movement of the spine, and for the spinal nerves to pass freely in and out of the spinal canal (see image below)
What causes degenerative disc disease?
When we are born, our discs are made up of approx 80% water, but as we age they lose fluid and dry out. This reduces the height and shock absorbing properties of the disc, leading to less padding and less space between the bones in the spine.
If the disc space is severely compromised it can cause more pressure on the bones (vertebrae) which can produce bony growths called bone spurs or osteophytes, eventually this can lead to osteoarthritis (also known as spondylosis). In some cases, the reduced space can also cause the spinal nerves to be pinched or irritated; depending on which area of the spine is affected, this may cause Cervical Radiculopathy (cervical spine) or Lumbar radiculopathy or “Sciatica” (lumbar spine) which typically produces symptoms of weakness, numbness, and hot, shooting pains in the arms or legs.
DDD also increases the risk of tears in the discs to develop, further compromising the disc space.
Risk Factors of Degenerative Disc Disease
While age is the biggest cause, other risk factors can speed up the process of degeneration or make you more at risk; these include:
- Obesity
- Heavy lifting or repetitive physical work
- Tobacco smoking
- An acute injury or previous fall, road traffic incident (RCI)
Secondary problems associated with degenerative disc disease
It is important to note that disc degeneration can also lead to or hasten the onset of other spinal conditions, such as:
- Herniated Disc: if the disc is compromised, it can bulge or herniate out through the fibrous outer portion of the disc.
- Spinal Stenosis: a form of spinal degeneration that leads to nerve root or spinal cord pinching.
- Spondylolisthesis: in which one vertebral body slips forward on another due to joint and disc degeneration.
- Degenerative Scoliosis: where discs and joints degenerate in a lopsided fashion and a ‘curve’ in the spine can develop over time.
These conditions can often have similar symptoms, therefore it is vital that you seek professional advice from an experienced healthcare professional, to get an accurate diagnosis.
What are the symptoms of degenerative disc disease?
The extent of the disc and joint breakdown and how it affects people varies hugely. One person may have severe disc damage on imaging, but only mild pain, while another may seemingly have minor disc changes but be in excruciating pain.

Degenerative disc disease typically consists of a low-level aching pain with intermittent episodes of more severe, stabbing/hot pain, plus or minus nerve symptoms affecting the arms or legs.
Symptoms Affecting the Lumbar Spine
- Lower back pain – Usually an ache with occasional sharp pains
- Pain can extend to legs and buttocks
- Feeling like your back has “seized” or “locked up”
- Worsens with twisting or bending
- Pain that worsens with extended periods of sitting
- Leg or foot weakness in severe cases
- Numbness or pins and needles in feet
Symptoms Affecting the Cervical Spine:
- Neck pain
- Pain extending from neck to shoulders and arms
- Numbness in arms or hands
- Symptoms worse when using a computer or sitting still
- Stiffness/loss of movement in your neck i.e difficulty looking over your shoulder.
- Weakness in arms or hands in severe cases
- Numbness or pins and needles in hands
How is degenerative disc disease diagnosed?
It can be quite difficult to diagnose degenerative disc disease because it develops so gradually and can have a multitude of related problems; for example, your physio may be able to quickly diagnose that you have sciatica or cervical radiculopathy, but it’s more challenging to diagnose that these issues are caused by degenerative disc disease. An MRI scan is required to confirm the diagnosis.
Complete Physio have highly specialised clinicians who are skilled diagnosticians, and will carry out an in depth and thorough assessment. Our physiotherapists can also refer you for an MRI scan if required. To make an appointment or to find out if we can help you, simply call 0207 482 3875 or email info@complete-physio.co.uk and our dedicated admin team will respond asap.
Medical History
Your physiotherapist at Complete Physio will listen and take a full account of your injury, asking a variety of questions about your general health, your past medical history, and what your normal daily activities and sports are. They will ask more specific questions about the location and type of pain you are experiencing and what other symptoms you have.
Physical Examination
They will then complete a thorough physical examination and a series of clinical tests to help develop a diagnosis. Depending on how severe your pain and symptoms are, your spinal physical assessment will also include assessing:
- Range of movement throughout your spine and pelvis
- Muscle strength of your lower legs or arm muscles
- Sensory and motor impairment
- Reflexes
- Spinal posture
- Pelvic and core stability
- The movement of the individual joints in the spine and surrounding structures, by gently and skillfully palpating the area.
- How you move or do certain activities, exercises or tasks
What imaging is required to diagnose Degenerative Disc Disease
It is important not to rely on imaging alone to diagnose DDD, as scan results only show a small part of the puzzle. A diagnosis must always be made by looking at the whole clinical picture, including the medical history and physical examination.
If your Physio feels that you require diagnostic imaging to help confirm their diagnosis or rule out other pathology, then they can refer you directly.
X-rays
X-rays cannot show soft tissue like discs, however they can show a decrease in the space between your discs, bone spurs (bony growths on your vertebrae), fractures, and other problems related to your bones.
MRI (magnetic resonance imaging)
An MRI scan is the imaging modality of choice to diagnose degenerative disc disease. This type of scan can provide a detailed image of your soft tissues. It can reveal if your discs have shrunk, if your spinal canal has narrowed, or if your spinal discs are damaged.
Computed Tomography (CT) Scan
These can provide a detailed image of bone structures in the spine and are useful if other pathology such as spondylolisthesis is suspected. It is also a useful option for those patients who cannot undergo an MRI (for example, those who have a pacemaker or a specific type of metallic implant).
How do we treat degenerative disc disease?
Physiotherapy
Physiotherapy should always be an essential part of conservative management for DDD. Depending on your symptoms and goals, there will be a number of treatment options for you that your physiotherapist will discuss with you, and together you will make an appropriate treatment plan.
Your treatment plan will likely combine pain relief techniques, mobility and stretching exercises, strengthening, core conditioning and posture/movement reeducation.
Pain Management
Initially your physiotherapy will focus on treatments to help settle your pain. Your physiotherapist will also give you advice on rest and activity modification, to reduce further flare ups while your pain subsides.
Medication
During this phase it is often useful to take a short course of medication to help manage your pain and symptoms. Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen can help to reduce swelling and inflammation of the joints and discs. If you are experiencing muscle spasms, a muscle relaxant may be prescribed, and if the pain is severe, a painkiller can also be taken with the NSAID or muscle relaxant. You must always seek professional advice from your GP, pharmacist or qualified prescriber before taking any medication.
Joint mobilisation and manipulation
These techniques are used by your physiotherapist, to restore full movement at each individual joint in your spine. Both techniques can significantly reduce tension in your muscles and significantly reduce your pain. Joint mobilisation is a gentle technique where your physiotherapist applies a slow movement to a spinal joint in a specific direction, A joint manipulation involves a small, rapid thrust to a specific joint in the spine to ‘unlock’ it and provide rapid pain relief and encourage movement at the joint.
It is characteristically, but not always, accompanied with an audible “click” or “pop” sound.
Soft tissue massage/release techniques
Massage is incredibly useful to help reduce tension and muscle spasms in the back and neck, to reduce pain and restore full range of movement in your spine.

Acupuncture or Dry Needling
There is good quality evidence to show that acupuncture is an effective treatment option for back and neck pain. Acupuncture has been proven to help with muscle spasm, improving blood circulation, regulating the nervous system, and releasing neurotransmitters to reduce pain. Many of our physiotherapists utilise acupuncture or dry needling as part of their treatment.
Restoring Movement and Strength
Once your pain has settled, it is important to get your joints and muscles moving. Our bodies are designed to be mobile, and complications can occur if we don’t start stretching and strengthening exercises as soon as possible.
Stretches
You will be given movement exercises to improve range of motion in your lumbar spine or neck. Depending on what was found during your physical examination, it may also be beneficial for you to stretch other areas of your body such as your pelvis, hips, shoulders or upper back.

Strength and Endurance
You will need to work on your postural and core strength. Your physiotherapist will commence you on a strengthening programme that specifically focuses on spinal stability, and exercises that target the deep postural muscles that dynamically control and stabilise your neck, or lower back and pelvis.
Your physiotherapist may also suggest that you commence a course of Pilates and rehabilitation, which is a highly effective way of managing mechanical low back pain and neck pain.
If you would like to learn more about the treatments we offer, please call 0207 482 3875 or email us info@complete-physio.co.uk
Functional and Posture Re-education
Your physiotherapist will assess the way you move and do functional tasks. Depending on your occupation, or chosen sport or activities, your physiotherapist will tailor your rehabilitation to work on specific actions and functional movements, to allow you to return to your desired activities and hobbies safely.
They will work on your sitting posture and movement patterns, and correct any abnormalities.
They can also carry out a full ergonomic assessment to review your working space if your symptoms are aggravated by sitting at work.
As your symptoms settle and you start returning to your normal daily activities, your Physiotherapist will work closely with you to ensure you have a long term management plan so that your symptoms don’t return.
They will make sure that you have a good understanding of your condition, and that you feel confident to self manage your symptoms and continue your exercises programme independently.
Spinal Injections for Degenerative Disc Disease
If after a number of physiotherapy sessions your symptoms are not settling, or if your pain is so severe that you are not able to engage in your rehabilitation programme, then spinal injections might be a good option for you.
Spinal injections are carried out with x-ray guidance, to ensure the correct disc or joint space is targeted. A mix of local anaesthetic and steroid is used, which can be very effective At Complete Physio we work with a number of highly regarded spinal specialists who can quarry out this procedure.
in reducing swelling and inflammation surrounding the injured disc, joint and nerve roots.
Injections should never be a stand alone treatment; the purpose of the injections is to provide a window of opportunity that enables the patient to completely engage in and benefit from a physiotherapy programme.
At Complete Physio we work with a number of highly regarded spinal specialists who can quarry out this procedure.
Surgery for Degenerative Disc Disease
Surgery is not often required, however if symptoms are severe and not settling with conservative management, then it may be an option. It is normally only considered if a patient is suffering from:
- Back or leg pain that stops the patient from carrying out normal daily activities
- Severe numbness or weakness in the legs or arms
- Difficulty standing or walking
- Pain affecting sleep
- Pain that is affecting a person’s mood and mental health
If a surgical opinion is required your physiotherapist will be able to refer you to one of the experienced Spinal consultants who we work closely with.
To make an appointment or to find out if we can help you, simply call 0207 482 3875 or email info@complete-physio.co.uk and our dedicated admin team will respond asap.
Don’t let pain hold you back, book now!




