
What is Spondylosis of the Spine?
Spondylosis is a type of degenerative arthritis that can cause loss of normal spinal structure and function due to ‘wear and tear’. It is important to remember that this happens to everyone’s spine to a more or lesser extent. Although ageing is the primary cause, the location and rate of degeneration, and how it impairs your movement and activities is individual. One of the biggest risk factors for you developing back pain are your genetics. Obviously this is not something we can change, but there are many other modifiable risk factors that we can influence to help reduce our chances of getting pain and reducing our pain if we already have it. These include our weight, activity levels, general fitness and stress levels.
The degenerative process of spondylosis mainly affects the vertebral bodies, the facet joints and the neural foramina (where the nerve roots exit the spine). It may affect the cervical (neck), thoracic (mid-back), or lumbar (low back) regions of the spine, although it is more common in the neck and lower back.

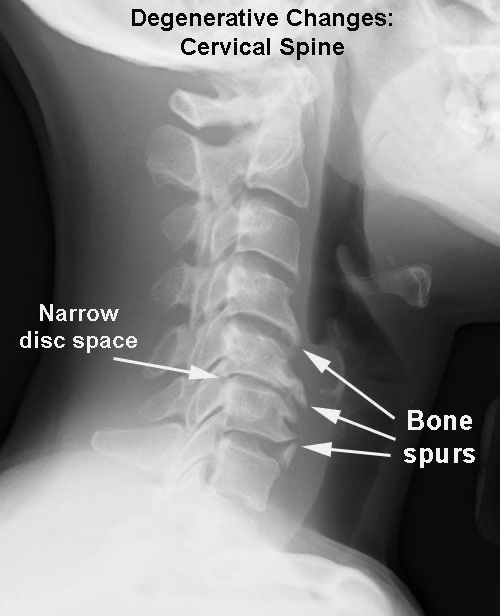
Degenerative osteoarthritis causes loss of joint cartilage i.e. the cushioning in the joints of the spine, and the formation of osteophytes i.e extra bits of bone called ‘bony spurs’. These bony changes can cause pain and inflammation, and if severe, can increase the pressure on the spinal cord or nerve roots, leading to altered sensation i.e. a change in the way your leg feels, motor impairments i.e. weakness in the leg muscles, and paresthesia, i.e pin and needles and numbness in your leg/foot.
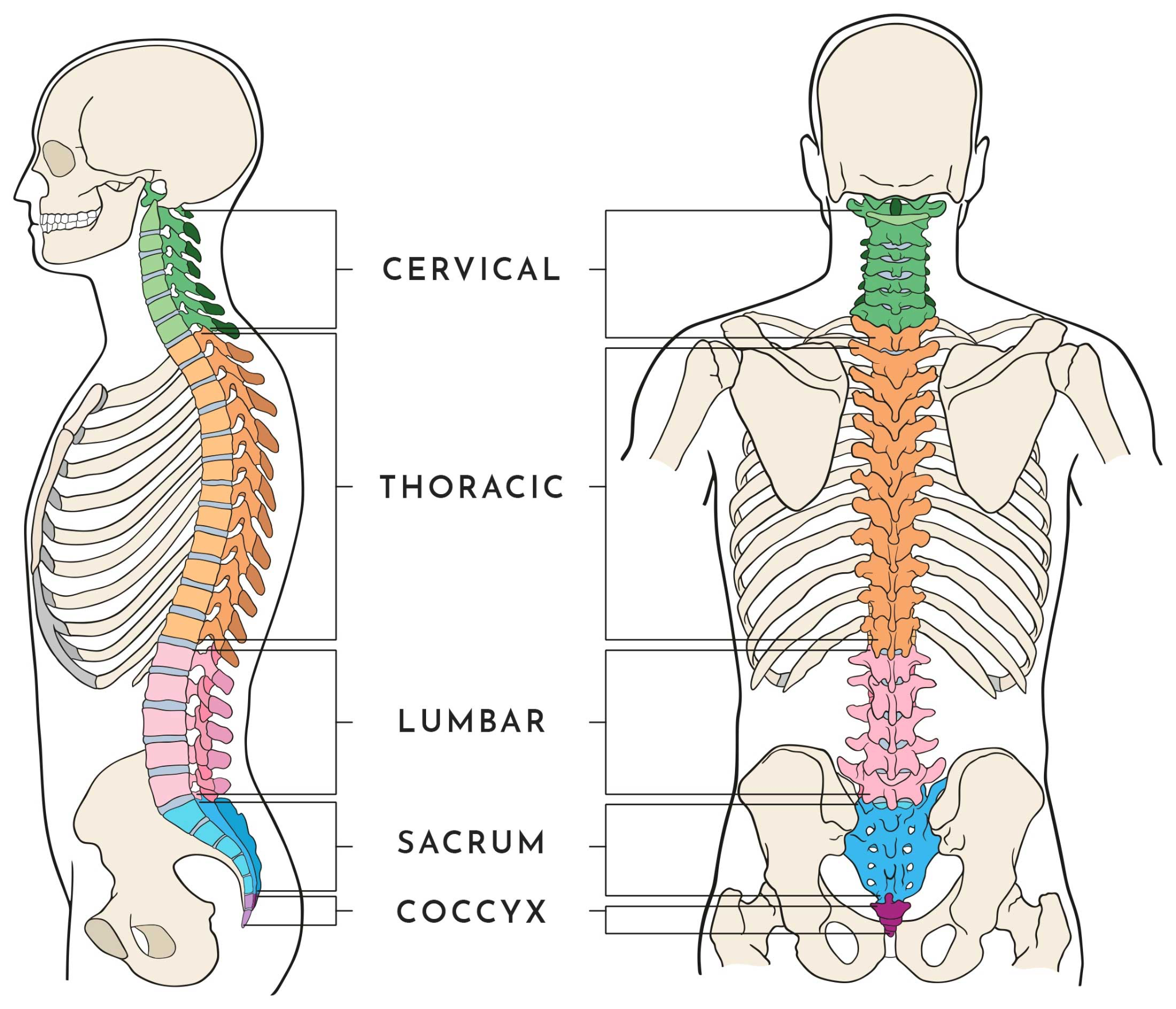
Your spine is what gives the body its structure; it’s made up of 33 moveable bones called vertebrae. These vertebrae are grouped into 3 sections called the cervical spine (neck), thoracic spine (upper back), and lumbar spine (lower back).
In between each vertebra is a spongy, shock-absorbing disc that adds cushioning and stability to the spine and prevents the vertebral bones from rubbing together.
Each vertebral body has four facet joints that work like hinges. These are the moving joints of the spine that allows the spine to flex (bend forwards), extend backwards, rotate (twist) and side flex (bend sideways).
Like other joints in the body, the bony articulating surfaces of the spinal joints are coated with cartilage. This cartilage is a special type of tissue that provides a self-lubricating and low-friction gliding surface.
The design of this structure ensures stability, flexibility and normal movement.
The spinal nerves exit just above the facet joint at each level of the spine, and provide sensory and motor control to the body.
What Causes Spondylosis?
Spondylosis is a condition that usually develops with age, and is the result of normal, daily “wear and tear” on both the soft structures and bones that make up the spine.
As people age, their vertebrae, facet joints, discs, cartilage, and ligaments change; the medical term for these age-related symptoms is Spondylosis.
Joint cartilage deteriorates on the vertebral bodies and facet joints (Lumbar or Cervical Facet Joint Pain), increasing friction between the joints which causes bone spurs (abnormal overgrowth of bones) to develop.
Vertebral discs become drier, thinner, and harder, and they lose some of their cushioning ability; this is known as Degenerative Disc Disease. This causes further friction on the joints and more osteophytes (bone spurs) to develop.
Degenerative changes may also cause the spinal ligaments to thicken and lose some of their strength, which leaves the joints at risk of excessive movement.
Risk Factors for Developing Spondylosis
We must remember you can have spondylosis and not have any pain. If we carried out an MRI scan of everyone over the age of 50, we would all have signs of spondylosis, because as we get older it is part of our normal ageing process, just like we all look different as we get older i.e we get “wrinkles” and our hair starts to thin and fall out!
However, as well as age, there are several factors that can predispose you to developing painful spondylosis.
These include:
- Genetics:
If you have a family history of spondylosis you may be more likely to suffer from this condition. - Repetitive Movement:
Repetitive strain on the spine from certain occupations or activities can contribute to the development of spondylosis. - Previous Trauma or Injury:
If you have sustained a previous injury to the spine, it can make you more predisposed to arthritic changes. - Smoking:
Cigarette smoking is known to increase the risk of developing chronic inflammatory changes in bone and soft tissue. - Obesity:
Increased BMI can put extra pressure on the joints and soft tissue in the spine, leading to more wear and tear.
- A Sedentary Lifestyle:
Lack of exercise can lead to weak spinal muscles. Without good muscle strength and support, increased forces are directed through the joints in the spine, again leading to an increased risk of arthritic changes. - Mental Health:
Having a mental health condition, such as anxiety or depression makes you at a higher risk of developing spondylosis. - Occupation:
Sitting for long hours at your computer, with a poor desk/ergonomic set up, tight deadlines, few breaks and minimal social interaction are all risk factors for developing back pain associated with spondylosis.
Symptoms of spondylosis at different spinal levels
As we discussed, having arthritic (spondylotic) changes in the spine doesn’t always result in pain or symptoms; many people have visible bony and joint changes on x-ray or MRI scans, and yet are non-symptomatic (pain free).
For the majority of people who have age related arthritic spinal changes, symptoms develop slowly over time. Common symptoms are feelings of stiffness, and mild to moderate dull aching pain that gets worse following certain movements or activities, or sometimes after periods of rest; such as after a long car journey or first thing in the morning. A majority of the time this is nothing to worry about and does not affect your ability to carry out the activities you enjoy.
Symptoms may vary depending on the location of the problem.
Cervical (Neck pain)
The neck produces a wide range of movement which can make it more susceptible to wear and tear, and degeneration.
In most cases the pain is localised to the neck initially, but if there are bony spurs or a disc prolapse or bulge (“a slipped disc” in layman’s terms) they can affect the adjacent nerve. This can cause pain and other symptoms such as pins and needles and numbness can radiate into the shoulders, upper back and even down the arm to the hand.
Common symptoms include:
- Localised neck pain at the level of the affected joint/joints
- Diffuse stiffness in the neck – difficulty moving your head
- Headaches
- Muscle soreness in the neck muscles.
- Pain radiating between the shoulder blades or upper back
- A feeling of weakness in the arm, wrist or hand
- Tingling, or a sensation of pins and needles in the arm and hand
Lumbar (Low Back)
Spondylosis in the lumbar spine is rarely seen in people under 40 and is more common in people over the age of 60. Depending on the severity of the condition one or more of the following signs and symptoms may occur:
- Localised dull back pain
- Stiffness which is typically worse in the morning
- Increased pain with prolonged sitting
- Increased pain with heavy lifting or higher impact exercise
- Referred or radiating pain into the buttock/back of the thigh
- A feeling of lower leg muscle weakness may also occur if the sciatic nerve is affected – this is usually only felt in one leg.
- Tenderness on palpation – increased pain when the area in the lower back is gently pressed.
- A feeling of grinding or grating in the back joints with movement (crepitus)
If you are suffering from any of the symptoms described above or have any concerns about back or neck pain, then please get in touch with us to book an initial assessment. You can call us on 0207 482 3875 or email info@complete-physio.co.uk and our dedicated admin team will respond asap.
How is Spondylosis Diagnosed?
Complete Physio have highly specialised clinicians who are skilled diagnosticians, and are experienced in treating patients with spinal conditions. Your Physiotherapist will carry out an in depth and thorough assessment to ensure an accurate diagnosis and can refer you for imaging tests if deemed appropriate. Please note most people do not require any imaging for us to be able to improve your pain and function.
X-ray. An X-ray can show changes in the spine, such as bone spurs (osteophytes), that indicate spondylosis. Neck X-ray can also rule out more serious causes for neck or back pain such as fractures or Spondylolysthesis.
MRI scan – an MRI can produce highly detailed images that can help pinpoint areas where nerves might be pinched such as discs and joints,
CT Scan – This test makes it easier to see the details of the spinal cord, spinal canal and nerve roots. A majority of the time a CT scan is not required.
If your Physiotherapist feels that you need an x-ray or scan, they will be able to refer you to an imaging clinic or specialist consultant.
How do we treat Spondylosis?
Most sufferers of this spinal condition will respond very well to physiotherapy and exercise-based treatment. Physiotherapy has been shown by research to reduce the pain and disability associated with spondylosis, and this should be the first line of intervention.
Unfortunately there is no cure for Spondylosis, however in the majority of cases physiotherapy treatment will significantly reduce your pain and provide you with the tools to manage any ongoing symptoms yourself, through activity modification and rehabilitation exercises.
At Complete Physio we use a variety of treatment options, from spinal manipulation to massage and acupuncture. The aim of treatment is to reduce your pain, improve your range of movement and can help slow down the speed with which your spondylosis deteriorates.
With the correct management you will be able to lead a very functional, less painful and highly enjoyable life, doing many of the activities that you normally do.
The aim of Physiotherapy is to:
- Relieve pain.
- Reduce muscle and joint stiffness.
- Strengthen your core muscles to stabilise the spine.
- Improve your quality of life and everyday living.
- Help you learn how to self manage your symptoms.
Your Physiotherapist will work closely with you to ensure your treatment is tailored to your individual needs and goals. Your treatment plan will likely include a combination of pain relief techniques, mobility and stretching exercises, muscle strengthening, core conditioning and posture/movement reeducation.
Pain Management
- Pacing
An important part of managing spinal conditions is ‘Pacing’, which ensures that you are able to maintain a healthy and active life, without overdoing it and having unnecessary flare ups of symptoms. Your Physiotherapist will offer you lots of advice on this aspect of pain management. - Medication
During the initial phase of your treatment, it is often useful to take a short course of medication to help manage your pain and symptoms. Common types of medications used for spondylosis are nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, painkillers and in more severe cases, corticosteroids. You must always seek professional advice from your GP, pharmacist or qualified prescriber before taking any medication. - Joint mobilisation and manipulations
These techniques are used to help restore full movement in your spine. Joint mobilisation and manipulation are effective ‘hands on’ techniques where your physiotherapist applies a movement to a spinal joint, which can significantly reduce tension in your muscles and help reduce your pain. All our physiotherapists at Complete are highly skilled and experienced manual therapists with many years of clinical experience.. They have all completed numerous hours of training at undergraduate and postgraduate level to ensure you receive the best level of care. - Soft tissue massage/muscle release techniques
Massage and soft tissue muscle release is a highly effective treatment modality to help reduce pain, tension and muscle spasms in the back and neck, and restore full range of movement in your spine.

- Acupuncture or Dry Needling
There is significant, high quality research that shows acupuncture can help with muscle spasm, improving blood circulation, regulating the nervous system, and releasing neurotransmitters to reduce pain; making it a very effective treatment option for back and neck pain. Many of our physiotherapists utilise acupuncture or dry needling as part of their treatment.
Restoring Movement and Strength
Once your pain has settled, it is important to get your joints and muscles moving. Our bodies are designed to be mobile, and complications can occur if we don’t start stretching and strengthening exercises as soon as possible.
- Stretches
You will be given range of movement and stretching exercises for your spine to improve your range and quality of movement. It may also be beneficial for you to stretch other areas of your body such as your pelvis, hips, shoulders or upper back. Your Physiotherapist will guide you through your individual programme during your treatment sessions, and will also give you some exercises to continue at home using our online exercise programme. - Strength and Endurance
Core strengthening exercises are a key component of treatment for spinal conditions; it is vital that you work on your postural and core strength. Your physiotherapist will teach you a strengthening programme that specifically focuses on spinal stability, and exercises that target the deep postural muscles that dynamically control and stabilise your neck, or lower back and pelvis. They will provide you with your own individualised rehabilitation programme using our online exercise system. 
Your Physiotherapist will also commence a strength programme with you which focuses on strengthening global muscles in the lower limbs, pelvis, shoulders and upper back.
For long term management, your physiotherapist may also suggest that you commence a course of Pilates and rehabilitation, which is a highly effective way of managing mechanical low back pain and neck pain.
- Functional and Posture Re-education
Your physiotherapist will assess the way you move and do functional activities so that they can tailor your rehabilitation to work on specific actions and functional tasks, to allow you to return to your desired activities and hobbies safely.
They will work on your posture and movement patterns, and correct any abnormalities.
They can also carry out a full ergonomic assessment to review your working space if your symptoms are aggravated by sitting at work.
If you would like to learn more about the treatments we offer, please call 0207 482 3875 or email us info@complete-physio.co.uk
As your symptoms settle and you start returning to your normal daily activities, your Physiotherapist will work closely with you to ensure you have a good understanding of your condition and how to self manage your symptoms and continue with your rehabilitation programme independently.
Things that you can do to self manage your symptoms:
- Pace yourself – rest when you have painful days and don’t over do it when you are feeling more pain free.
- Maintain a good level of general fitness within your limits of symptoms – lower impact cardiovascular exercises such as walking, cycling and swimming are best.
- Avoid heavy lifting or overstressing your joints with high impact exercises.
- Maintain a healthy BMI – being overweight will increase the stress going through your joints
What if your pain is not improving?
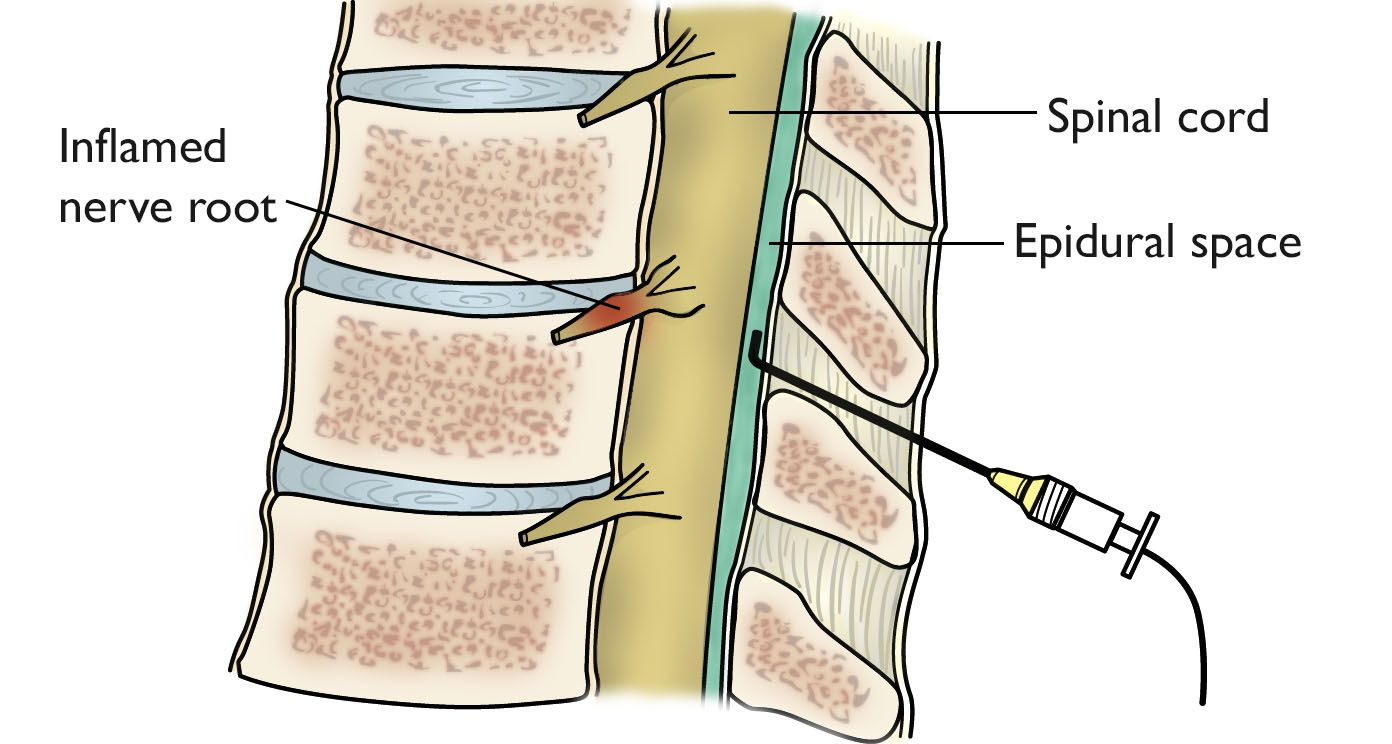
If conservative treatment is not settling your symptoms, it may be appropriate for you to have a spinal injection to directly target the source of your pain.
Epidural Steroid Injection
This is one of the most common injections as it’s especially effective for low back pain caused by the issues related to spondylosis.
An epidural steroid injection targets the space surrounding the membrane that covers the spine and nerve roots (the epidural space). A mix of local anaesthetic and steroid is used, which is very effective in reducing swelling and inflammation surrounding the injured spinal joints, discs and nerve roots. They are more commonly carried out the the lumbar and cervical region of the spine, but can also be used for thoracic pain when appropriate.
Facet Joint Injection
Also known as facet joint blocks; these injections are useful if your facet joints are the structure causing pain – as they often are in spondylosis. Again, a mix of steroid and anaesthetic is used, this time targeting the spinal facet joints. A facet joint injection will numb the joint, reduce inflammation, and can significantly reduce your pain caused by spondylosis
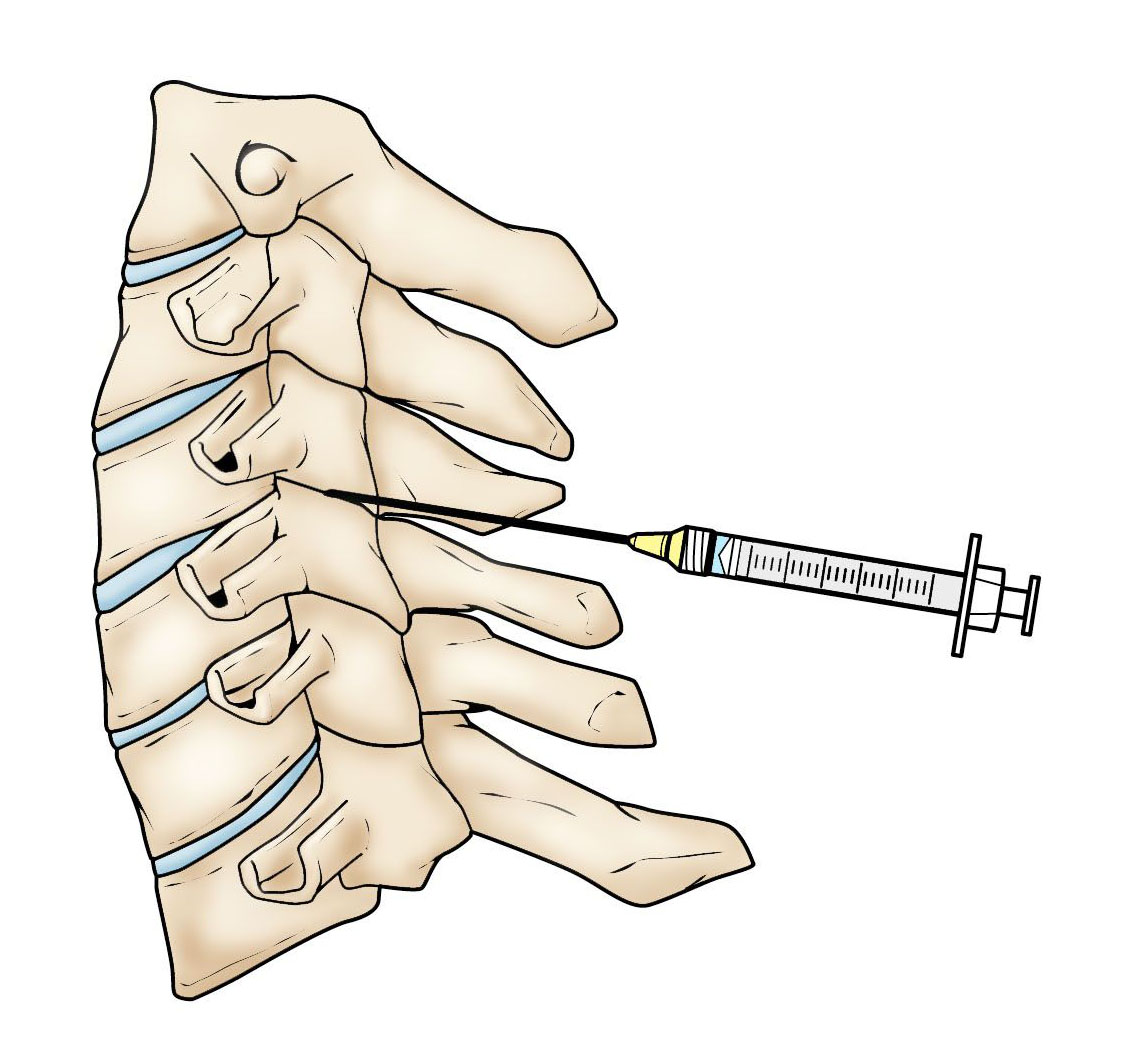
The main goal of corticosteroid injections is to manage pain caused by irritation and inflammation. Having significantly less pain will promote normal movement and function; this provides a window of opportunity that enables the patient to completely engage in and benefit from a physiotherapy programme.
Spinal injections are quite complex and precise, and therefore should only be performed by a healthcare provider with significant specialised training.
At Complete Physio we work with a number of highly regarded spinal, and pain specialists who can quarry out this procedure. We ensure that we regularly communicate with you and your specialist, and take a multidisciplinary approach to your care to optimise your recovery.
Surgery for Spondylosis
When symptoms of Spondylosis persist or worsen despite conservative treatment, you may require a surgical referral to a spinal consultant to discuss surgery options.
The goal of surgery is to relieve symptoms by decompressing, (relieving pressure) on the spinal cord. This will likely involve removing the pieces of bone (bone spurs) or soft tissue (herniated disk or thickened spinal ligament), that are narrowing the spinal canal, therefore creating more space for the spinal cord and relieving your symptoms.
The other type of surgery that is commonly used to treat Spondylosis, is a Spinal Fusion. This operation stabilises the spine by permanently joining two vertebrae together, eliminating movement between them. This is the preferred procedure for spondylolysis in older patients.
Spinal surgery is usually reserved for patients who have progressive neurological changes such as:
- Disabling pain
- Severe weakness in the arms or legs
- Significant numbness in hands or feet
- Balance and gait issues
- Bilateral symptoms
- Symptoms affecting bladder and bowel function
Complete Physiotherapy has an excellent reputation within orthopaedic and musculoskeletal healthcare, and we work with some of the best consultants in the country. If an onward referral is required, we will make sure that you receive exceptional care from a trusted and highly regarded spinal consultant.
To make an appointment or to find out if we can help you, simply call 0207 482 3875 or email info@complete-physio.co.uk and our dedicated admin team will respond asap.
Don’t let pain hold you back, book now!





