What is an anterior cruciate ligament (ACL) injury?
An ACL injury is a sprain or tear of the anterior cruciate ligament (ACL). The ACL is a very strong band of soft tissue that helps connect your thigh bone (femur) to your shinbone (tibia). There are two cruciate ligaments in the knee’ the ACL and the PCL (posterior cruciate ligament). ACL injuries are far more common than PCL injuries.
ACL injuries most commonly occur during sports that involve powerful acceleration and deceleration, sudden changes of direction, or jumping and landing – such as football, rugby, hockey and skiing. If the stress placed on the ligament exceeds the tensile strength of this structure, this will lead to either a ‘partial’ or ‘full’ tear (also known as a ‘complete’ tear or ‘rupture’ of the ligament fibres.
Of the four major knee ligaments, an ACL rupture is the most debilitating knee ligament injury. While you may be able to function in your normal daily activities without an intact ACL, competing in high-demand sports may prove difficult and ACL injuries can curtail many promising sporting careers.
About half of all injuries to the anterior cruciate ligament occur along with damage to other structures in the knee, such as articular cartilage (which can cause osteoarthritis), meniscus, or other ligaments.
Injured ligaments are considered “sprains” and are graded on a severity scale.
Grade 1 – The ligament is mildly damaged in a Grade 1 Sprain. It has been slightly stretched but is still able to help keep the knee joint stable. grade 2 injuries represent the partial tears
Grade 2 – A Grade 2 Sprain stretches the ligament to the point where it becomes loose. This is often referred to as a partial tear of the ligament. Grade 2 injuries represent the ‘partial’ tears.
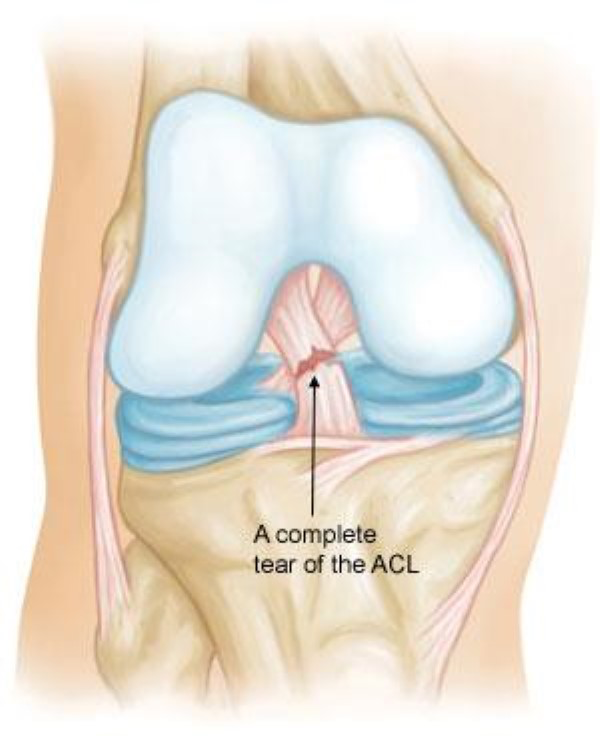
Grade 3 – This type of sprain is most commonly referred to as a full/complete tear or rupture of the ligament. The ligament has been split into two pieces and the knee joint is unstable.
Partial tears of the anterior cruciate ligament are rare; most ACL injuries are grade 3 complete tears.
Anatomy
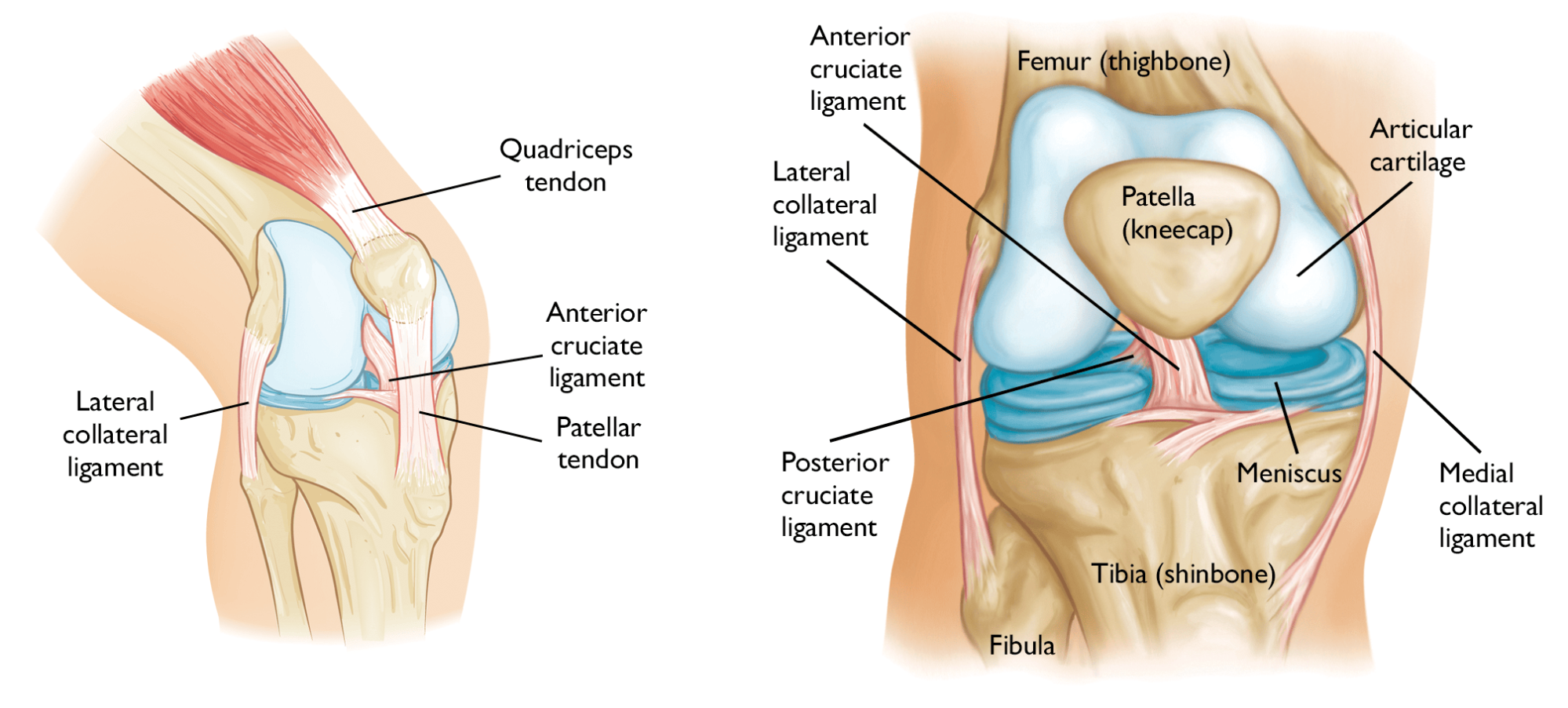
The knee is made up of the femur (thigh bone), the tibia (lower leg bone), and the patella (kneecap). (See images below).
The knee is essentially a hinged joint that is held together by the four main ligaments which attach to the bones and act like strong ropes, holding the bones together.
The weight-bearing surface of the knee is covered by a layer of articular cartilage. On either side of the joint, between the cartilage surfaces of the femur and tibia, are the medial meniscus and lateral meniscus. The menisci act as shock absorbers and work with the cartilage to reduce the stresses between the tibia and the femur.
Collateral Ligaments
These are found on the sides of your knee. The medial collateral ligament (MCL) is on the inside and the lateral collateral ligament (LCL) is on the outside. They control the sideways motion of your knee and brace it against unusual movement. The MCL ligament is often injured at the time of an ACL injury.
Cruciate Ligaments
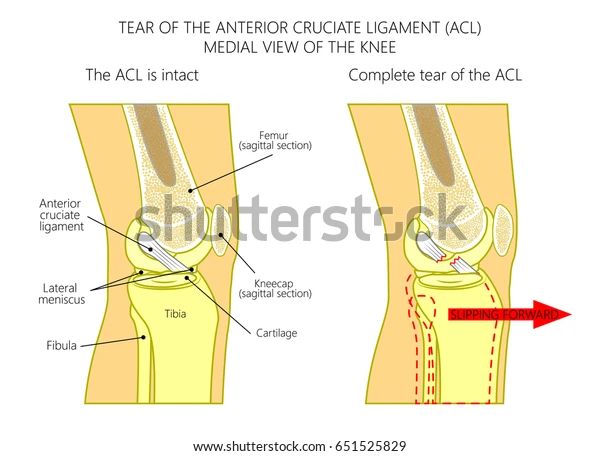
These are found inside your knee joint. They cross each other to form an “X” like a crucifix, with the anterior cruciate ligament (ACL) in front and the posterior cruciate ligament (PCL) behind. The cruciate ligaments control the back-and-forth motion of your knee.
The ACL runs diagonally in the middle of the knee. It prevents the tibia from sliding out in front of the femur, and also provides rotational stability to the knee.
As well as giving the knee stability the cruciate ligaments provide an even more vital role; over recent years researchers have found that the cruciate ligaments contain tiny cells called ‘proprioceptors’, these cells provide sensory feedback to the brain, so that your brain knows where your knee is in relation to your body and to the ground, and what position the knee is in. Proprioception is closely tied to the control of movement and balance which is essential to help with injury prevention.
What causes an anterior cruciate ligament (ACL) injury?
ACL injuries often happen during sports and fitness activities that put stress on the knee. A valgus force is placed onto the knee joint causing the knee to twist and injure the ACL.
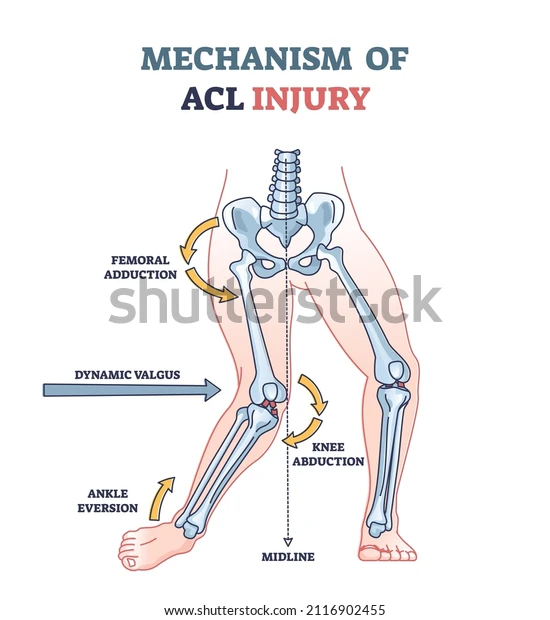
The ligament can be injured in several ways:
- Suddenly slowing down and changing direction (cutting).
- Pivoting with your foot firmly planted.
- Landing awkwardly from a jump.
- Stopping suddenly.
- Receiving a direct blow to the knee or having a collision, such as a football or rugby tackle.
Most ACL tears occur from a non-impact injury.
Risk Factors
There are a number of factors that increase your risk of an ACL injury, including:
- Sex – women are at higher risk of sustaining an ACL injury. This is thought to be due to either differences in anatomy, muscle strength, or hormonal influences, or possibly a combination of these.
- Participating in certain sports, such as football, rugby, basketball, netball, gymnastics, skiing.
- Poor strength conditioning.
- Poor lower limb biomechanics.
- Wearing poorly fitting footwear.
- Using poorly maintained sports equipment, such as ski bindings that aren’t adjusted properly.
- Playing on artificial turf or harder surfaces.
What are the symptoms of an anterior cruciate ligament injury?
When you injure your anterior cruciate ligament, you might hear a “popping” noise and you may feel your knee give out or give way from under you, causing you to fall on the floor.
Other typical symptoms include:
- Severe pain and inability to continue activity
- Swelling – usually the knee will swell within 24 hours of the injury
- Loss of full range of movement of the knee
- A feeling of instability and/or weakness and the knee giving way
- Tenderness along the joint line
- Discomfort while walking.
If you are experiencing any of these symptoms, or suspect that you have an ACL injury it is essential to get the correct diagnosis asap to avoid long term knee damage. To see one of our expert physiotherapists, please call 0207 482 3875 or email info@complete-physio.co.uk. If you would like to speak to a specialist before booking, then please send us an email with your details and we will call you back.
How is an anterior cruciate ligament injury diagnosed?
Obtaining an accurate diagnosis is essential; it allows the clinician to select the most effective treatment plan for you. Your physiotherapist at Complete will firstly ask specific questions about your injury, past health, symptoms, and exercise regime.
The mechanism of injury and a description of symptoms often gives the clinician a clear hypothesis for your potential diagnosis.
After this history taking, your physio will complete a series of clinical tests to help confirm a diagnosis. Depending on the severity of your symptoms, these may include:
- Measuring the range of movement of your knee.
- Assessing muscle strength, particularly the quadriceps at the front of your thigh, and also the muscles around your lower leg and hips.
- Assessing muscle length and flexibility of quadriceps, hamstrings and calves.
- Watching you move your knee and how you perform activities such as squatting, hopping, jumping, running.
- Gently, but skilfully, feeling around your knee joint to find exactly where it is most painful.
- Functional tests – if your pain is present during a specific activity or task, you may be asked to perform these, so the physiotherapist can assess exactly what is aggravating your pain.
- There are specific ACL tests called a Lachman’s test, pivot shift test and an anterior drawer test that your physiotherapist may carry to assess if the ACL is intact. With the Lachman’s and anterior drawer test, if the ACL is torn, the examiner will feel increased forward (upward or anterior) movement of the tibia in relation to the femur (especially when compared to the uninjured leg), and a soft endpoint when this movement ends.
Will I need a scan?
Although clinical assessment is very reliable for diagnosing an ACL tear, an MRI scan is usually required to confirm the diagnosis and assess from any other injuries such as a bony injury or a meniscal tear. If pain and swelling are significant symptoms, then a full, clinical examination may be quite limited and an MRI will certainly be required.
MRI
MRI is the gold standard imaging to confirm an ACL tear. An MRI uses radio waves and a strong magnetic field to create images of both hard and soft tissues in your body. If we are unsure of your diagnosis or we would like to understand more about the extent of the ligament tear, then we may refer you for an MRI scan. MRI scans can also be useful to check for evidence of injury to the other knee ligaments, the menisci, or the articular cartilage. We can refer you directly without going to your GP.
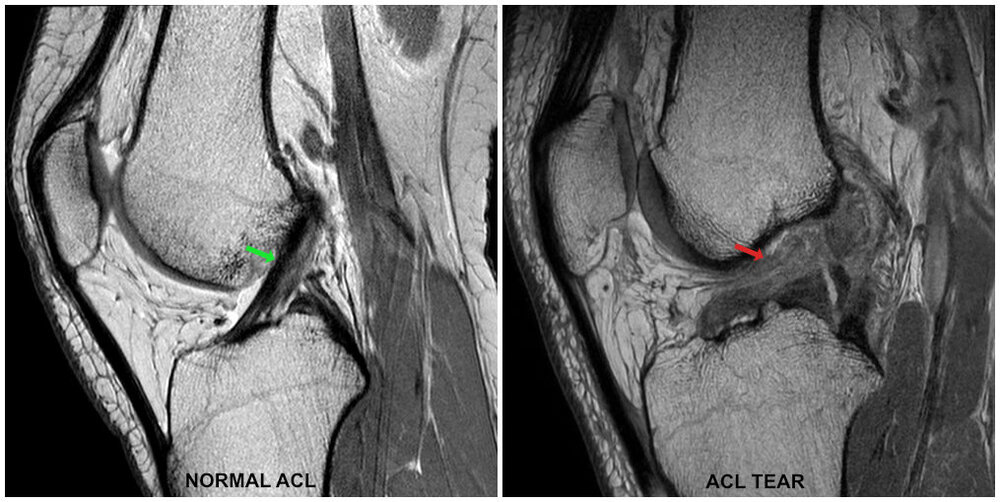
The MRI on the left shows a normal ACL, whereas on the right there is an ACL tear, as you can no longer clearly see the ligament.
Diagnostic Ultrasound Scan

Whilst ultrasound is not typically used to assess the ACL in the knee, it can be used to assess other structures such as the two collateral ligaments and parts of the meniscus, which are often damaged alongside the ACL. It can also be used to assess the extent of any knee effusion (swelling inside the joint), and any related tendon or muscle issues.
At Complete Physio, many of our clinical specialist physiotherapists are also fully qualified musculoskeletal sonographers and will carry out a diagnostic ultrasound scan of your knee as part of your assessment (please request when booking if you would like to have a diagnostic ultrasound as part of your assessment).
X-rays
Although they will not show any injury to your anterior cruciate ligament, x-rays can show whether the injury is associated with a broken bone.
How do we treat anterior cruciate ligament injuries?
An ACL injury is often seen as a devastating injury, with treatment decisions frequently made early after injury, regularly favouring surgery. But not everyone has to have surgery after an ACL injury. At Complete Physio we have seen many patients with ACL ruptures return to full sport including football and skiing!
No matter whether you have surgery or not, everyone who has injured their ACL should have a structured rehabilitation program. Management and treatment of your ACL injury will depend on a number of factors including:
- Your age.
- Whether you have a full or partial ACL tear.
- Your current level of activity/sport and your future sporting plans.
- The type of activity/sport you take part in – more rigorous, high-demand sports that involve a lot of “cutting”, twisting and pivoting are much more reliant on an intact, functioning ACL.
- Your level of knee instability – whether you have positive clinical signs of instability, and also whether your knee feels unstable (gives way) during daily activity/exercise.
- Whether there are other structures damaged such as your meniscus or collateral ligaments.
There are usually three ACL treatment options:
- Non-surgical management
Initially, the goal of rehabilitation is to reduce pain and swelling, restore your knee’s full range of motion, regain proprioception and stability, and strengthen muscles.There is some evidence that shows the ACL can reattach to surrounding structures after a few weeks, giving the knee a good level of stability, therefore you may be required to wear a knee brace for a few weeks to offload the ligaments and give them time to heal. This course of conservative management is often very successful in treating patients with a grade 1 or a grade 2 (‘partial’) ACL tear, even if you want to return to high speed, dynamic sports such as football, skiing and rugby. Individuals who are relatively inactive, only engage in light exercise and recreational activities, and/or play sports that put less pivotal stress on the knees such as cycling or running are unlikely to require surgery.Your physiotherapy treatment will aim to:
This course of conservative management is often very successful in treating patients with a grade 1 or a grade 2 (‘partial’) ACL tear, even if you want to return to high speed, dynamic sports such as football, skiing and rugby. Individuals who are relatively inactive, only engage in light exercise and recreational activities, and/or play sports that put less pivotal stress on the knees such as cycling or running are unlikely to require surgery.Your physiotherapy treatment will aim to:
- Reduce pain and inflammation
- Regain full joint range of movement
- Strengthen your knee, lower limb and pelvis
- Improve patella (kneecap) alignment
- Normalise your muscle lengths
- Improve your proprioception, agility and balance
- Improve your technique and function
- Minimise your chance of re-injury.
At Complete Physio we are highly experienced in treating ACL injuries, and your physiotherapist will take you through a specific, tailored ACL rehabilitation programme, which may include:
- Relative rest – advice on rest and activity modification allowing the pain and swelling to settle down and the ACL to heal appropriately.
- Patient education – it’s important to understand your condition and to be active in your recovery. You will be given a clear explanation of the diagnosis and any other underlying causes, and we will discuss what is required to address these issues and reach your goals.
- Pain and swelling management – ice can be applied to the affected area to help with pain and swelling. Painkillers and anti-inflammatory medication are often useful in the early stages of management (any medication needs to be approved by a pharmacist or doctor)
- Range-of-movement exercise – your physiotherapist may teach you self-stretching methods. These can decrease tension and help restore normal movement of your injured joints.
- Manual therapy – Your physiotherapist may use manual therapy such as massage or soft tissue release techniques to the surrounding muscles and joint mobilisations. This will help improve joint movement and reduce muscle stiffness or soreness.
- Specific strengthening exercises – the muscles around your knee will need to be very strong in order to compensate for the reduced stability from your ACL. Your physiotherapist will design a safe resistance program to ensure all your muscle groups (especially your quadriceps and hamstrings) are strong and working in synergy, to aid your recovery and prevent recurrence of injury. This is a key component of your treatment programme and requires commitment and consistency.
Can u use the image of me and helen on leg press – here
- Proprioception and balance exercises – these exercises help your brain to reconnect with your knee, so that you know where your knee is in space and in relation to other parts of your body during movement. Not only is this important for regaining full function after ACL injury, but also for the prevention of further ACL injuries.
- Biomechanical and movement re-education – this may involve teaching you how to correctly squat, run or jump.
- Functional and sport-specific training – once your pain, strength, and range of movement improve, functional and sport-specific training can help you safely resume more demanding activities and sports.
Throughout your treatment at Complete Physio, we will keep revisiting your personal goals, so that we maintain the focus on making your life easier and ensuring that you feel supported and involved in your rehab process. As part of the rehabilitation program, we also conduct regular clinical testing to ensure that you are on track with your recovery to achieve your goals.
At Complete Physio we have successfully rehabilitated Olympic athletes, professional and elite level sportsmen and women and got them back to sport safely and in the shortest time frame possible.
- Early surgical reconstruction
This option is appropriate if you are an athlete and want to continue to an elite level in your sport, especially if the sport involves jumping, cutting or pivoting. It is also a good option for grade 3 complete tears, especially if more than one ligament or the meniscus in your knee is also injured, as delayed surgery can sometimes lead to further damage to these structures.It is important to note that even with early surgical management, your surgery will not likely take place until you have regained a good range of movement in your knee and the swelling has significantly reduced. You will therefore be required to undergo prehabilitation with your physiotherapist for a number of weeks, to get you ready for reconstructive surgery. - Delayed surgical reconstruction
Evidence currently demonstrates that undertaking a rehabilitation programme and delaying a decision regarding surgical intervention for approximately 3 months, may have the best long-term outcome in recreationally active individuals who take part in moderate to high levels of activity/sport. This management approach is often taken if there is an isolated ACL injury (partial or complete), and if the individual is not experiencing significant instability with normal daily activities.An intensive course of physiotherapy and close follow up is vital to identify any ongoing knee instability, and whether surgery is likely to be required.The decision on how your ACL injury is managed will be discussed with you at length and you will be given all the relevant and appropriate information to make an informed decision. Your physiotherapist will work together with your consultant to help guide you through the process.At Complete Physio we work with some of London’s most highly regarded and experienced orthopaedic surgeons. If an onward referral is required, we will ensure that you are provided with the best care possible and will continue to support your recovery every step of the way.
What is ACL reconstruction surgery?
During ACL reconstruction, the surgeon removes the damaged ligament and replaces it with a segment of tendon – tissue similar to a ligament that connects muscle to bone. This replacement tissue is called a graft.
Your surgeon will use a piece of tendon from another part of your knee (usually your hamstring), or a tendon from a deceased donor.
The surgery is performed arthroscopically i.e., keyhole surgery with small incisions and with minimal damage to other tissue or structures.

After surgery you will be referred back to your physiotherapist at Complete to resume a course of post operative rehabilitation. Successful ACL reconstruction surgery, paired with rigorous and specialised rehabilitation, will give you the best outcome to restore the stability and function of your knee, and get you back to the sport and activities that you love.
It can be a long road to recovery after an ACL injury, regardless of whether it is managed conservatively or surgically. At Complete Physio we are committed to getting you back to full function and we have the skills and knowledge within the practice to ensure this goal is achieved.
If you would like to book an appointment or speak to one of our expert physiotherapists about your knee, please call 020 7482 3875 or email info@complete-physio.co.uk.
Don’t let pain hold you back, book now!




