What is Cervical Radiculopathy?
Cervical radiculopathy occurs when a nerve in the neck is compressed, damaged or irritated as it exits the spinal column. It is commonly known as a “pinched nerve”, and usually causes pain that radiates into the shoulder and/or arm, and can also result in symptoms of muscle weakness and numbness.
Most of the time cervical radiculopathy appears unilaterally (on one side of the body), however it is possible for bilateral symptoms (on both sides of the body) to be present if there is more severe compression or irritation of the nerve root on both sides of the neck.
The purpose of this article is to provide information and advice on:
- The anatomy of the cervical spine and radiculopathy.
- The common causes and risk factors of cervical radiculopathy.
- What the signs and symptoms are.
- How we diagnose the condition.
- What treatments are available to you.
Anatomy
The spine is an immensely complex structure! Your spine is made up of twenty four vertebral bones that are stacked together to make the spinal column. The first seven vertebral bones are called the cervical spine, which starts just below the skull and forms the neck.
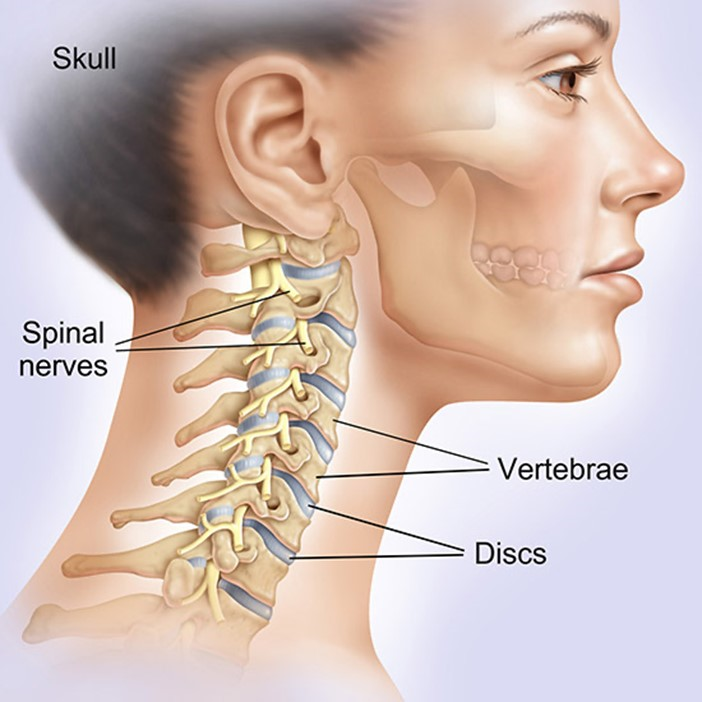
Between each vertebrae are intervertebral discs which act as shock absorbers, and protect your neck joints. This shock absorbing mechanism also reduces the vibrations and forces going through your skull when we walk or run, helping protect your brain.
The cervical spine is much more mobile than the thoracic and lumbar regions; it allows your head to move in nearly every direction. Unfortunately this level of flexibility often makes it more susceptible to injury.
The vertebral column also houses and protects the spinal cord, and at each vertebral level, nerve roots branch out from the spinal cord through openings in the vertebra called the foramen. It is the nerve roots that get “pinched” or irritated, which causes Radiculopathy.
There are eight pairs of cervical nerve roots (C1 – C8), in the cervical spine. Once these cervical nerves exit the spine, they branch out further to supply your muscles that enable movement and function of the shoulders, arms, hands, and fingers. They also carry sensory nerve fibres to the skin that provide sensation.
What Causes Cervical Radiculopathy?
Radiculopathy is typically caused by damage or changes in the structures surrounding the nerve roots. These can include bones of the spinal vertebrae, intervertebral discs, or less commonly, the tendons and ligaments along the spine. In most cases, these changes are caused by gradual degeneration that happens as you age, but it can also be a result of injury or acute spinal damage or injury.
Bone Spurs
With the natural ageing process, our joint cartilage deteriorates (Osteoarthritis of the Spine) which adds an increased stress directly on the bones and joints in our spine. Small areas of extra bone (bone spurs) can develop around the spinal joints, specifically the Facet Joints and Foramen, where the nerve roots exit the spinal column. These areas of extra bone growth can compress or irritate the nerves leading to symptoms of Cervical Radiculopathy.
Herniated Discs
Another cause of Cervical Radiculopathy is a bulging or herniated disc (when the soft cushion of tissue between the bones in your spine pushes out).

As previously mentioned, Spinal Discs act as cushions between your vertebrae. As we age, these discs become slightly worn and can slip out of place or become damaged (Degenerative Disc Disease) and press on the nerves. Pressure against the nerve root can cause pain, numbness and weakness along the area the nerve supplies. It is also thought that chemicals released from the damaged disc can add to the symptoms, especially pain.
A herniated disc can also happen as a result of a direct injury or trauma, such as a fall, sports injury or car accident, rather than from wear and tear. This problem is more likely to occur in your lower back, but it can also affect your neck.
Other, less common causes:
- Thickening of the spinal ligaments due to degeneration or injury may also lead to narrowing of the space around the nerve roots and subsequent nerve compression.
- Cancerous and noncancerous growths in the spine that may press against the nerve roots.
- Spinal infections causing inflammation of the nerves.
Anyone can get cervical radiculopathy, but it’s more common in adults.
People in their 20’s/30’s tend to get cervical radiculopathy from sports injuries and trauma, while people in their 50s/60s are most likely to be affected by a degenerative, or herniated disc. In patients over 60, symptoms are highly likely to be caused by joint changes and bone spurs.
These symptoms can also be linked to arthritis of the spine (Spondylosis), which is why it is vital that you see an experienced healthcare professional to ensure you get an accurate diagnosis.
What are the Symptoms of Cervical Radiculopathy?
The main symptom of cervical radiculopathy is pain in the neck that spreads into the arm, chest, upper back and/or shoulders. Often, the pain in the neck is more mild than the pain and symptoms felt further down the nerve into your arm.
Compression of the nerve can also lead to sensory issues, such as numbness, tingling or pins and needles in your fingers and hand; and/or motor problems such as muscle weakness in the arm or hand, reduced coordination or loss of upper limb reflexes.
These symptoms can be confusing and disconcerting, as although the problem is in the spine, the symptoms are felt in the area of the upper limb where the nerve supplies and travels. The good news is that by looking at the specific patterns and areas where the symptoms are, your spinal specialist can usually tell which nerve is involved.
Below is a diagram of where each cervical nerve runs through the upper limb, and which areas might be affected by symptoms such as pain, numbness or muscle weakness.
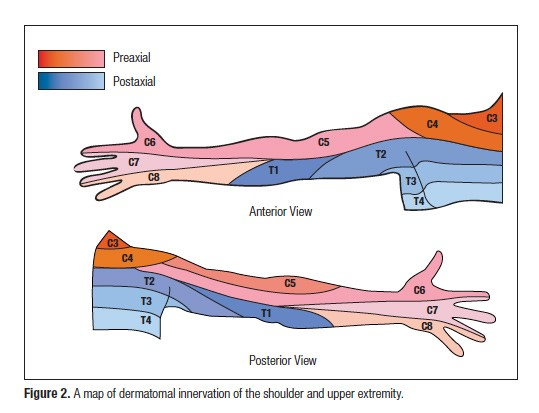
Cervical radiculopathy signs and symptoms most commonly appear gradually and intermittently at first; coming and going with certain activities or movements. As the problem progresses, they can become more constant and episodes last longer. Due to the nature of nerves, they can be quite easily flared up, but can take much longer to settle down! Symptoms are mostly seen unilaterally (on one side) but can affect both sides (bilateral) in severe cases.
People with cervical radiculopathy typically describe the pain as a sharp or burning pain.
Common Symptoms of Cervical Radiculopathy include:
- Pain in the neck.
- Pain in the arm, chest, upper back and/or shoulders.
- Tingling or the feeling of “pins and needles” in the fingers or hand.
- Weakness in the muscles of the arm, shoulder, or hand – this often presents as a weak hand grip or dropping things.
- Loss of sensation and numbness in the hand or arm.
- Muscle spasms or tightness.
- Headaches – especially in the back of the head.
How do we Diagnose Cervical Radiculopathy?
Subjective Medical History
In most cases a diagnosis of cervical radiculopathy is primarily made based on the patient’s symptoms, a good medical history of and thorough physical examination.
The more information you can tell your Physiotherapist about your symptoms and your aggravating and easing factors the better; from a detailed subjective history your Physio will be able to create a hypothesis on what your problem is, and they will then carry out a full physical examination to confirm their diagnosis.
Physical Examination
Using their professional skills, your Physiotherapist at Complete will assess each level of your spine and confirm the specific nerve that is causing the problem, and what the underlying pathology is likely to be.

Your spinal physiotherapist, will expertly assess your neck and upper limbs; the physical examination will likely include assessing:
- Range of movement of your neck and shoulders
- Muscle strength of your neck, arms and hands
- Testing signs for nerve tension and irritation – nerve tension tests
- Sensory impairment throughout your upper limbs
- Upper limb reflexes
- Spinal posture
- Cervical spinal stability and neck control
- Muscle spasm and muscle tightness
Will I Need a Neck Scan?
Imaging studies are not usually required, however scans such as X-ray, or MRI, may be ordered if your therapist suspects there may be other spinal issues, or to assist with a more complex diagnosis.
X-Rays
X-rays show the bones of the cervical spine, but do not show the soft tissue structures such as the nerves, discs, and muscles. They can show bony problems such as fractures, infection, or tumours of the bones. X-rays can also be useful to give some idea of how much degeneration has occurred in the spine; the narrowing of the disc space between each vertebrae and bone spurs show up on x-ray.
Magnetic Resonance Imaging (MRI)
MRI is the most commonly used test to evaluate the spine because in addition to the bones, it can also show 3D images of the nerves and discs.
It is really important to note that imaging can often over diagnose, and therefore your physiotherapist will look at the whole clinical picture; guided mostly by your symptoms and their physical examination when giving you a diagnosis and planning your treatment pathway.
If your Physiotherapist feels that you need a scan, they will be able to refer you to a specialist spinal consultant or clinic.
How is Cervical Radiculopathy Treated?
Complete Physio has gained an excellent reputation as one of the leading Physiotherapy practices in London. We have a number of highly specialised Physiotherapists who have years of experience and expertise treating patients suffering with spinal conditions, and we are trusted by some of the most highly regarded spinal surgeons and sports medicine consultants in the country to treat their patients
From your clinical assessment, your physiotherapist at Complete Physio will go through the main causes of your symptoms and provide you with a tailored regime based on your individual needs and goals.
There are three main aspects to your treatment:
- Reducing your pain and symptoms
- Restoring movement and function
- Reducing the risk of recurrence/reinjury
Your treatment programme at Complete Physio will often include some or all of the following:
Information and Education
We will ensure that you have a clear understanding of your condition and what is causing your problems. Your physiotherapist will answer any questions and concerns that you have, and will make sure that you know what will be required to progress and optimise your recovery.
Pain Control
Pain is often the reason why people eventually seek professional advice. Reducing your pain and symptoms is a huge priority in the initial phases of treatment. Being more pain-free will allow you to properly engage in your rehabilitation; it will also enable you to move more normally, be more active, and will have a positive effect on your sleep – which is vital for tissue repair and healing.
Your physiotherapist will use various treatment tools to help reduce your pain, inflammation and muscle spasm; these include ice/heat, acupuncture, soft tissue massage, joint mobilisations and taping to offload injured structures.
Medication
You may also benefit from taking a short course of medication to help manage your pain and symptoms.
The most common kinds of medications that are prescribed to help control symptoms of cervical radiculopathy include painkillers, nonsteroidal anti-inflammatory drugs, muscle relaxers and drugs that reduce neuropathic pain. You should always seek medical advice before taking any medication.
Manual (hands-on) Physiotherapy
Your physiotherapist may use hands-on therapy, such as manual cervical traction or joint mobilisations to help relieve pressure in the neck area. Traction can help provide immediate relief from pain and arm numbness. Your physical therapist also may gently massage the muscles of your cervical spine and shoulder blade area to reduce tension and muscle spasm associated with this condition.
Movement, Muscle Strength and Function
Once your pain has settled, the next phase is to work on regaining your movement and muscle strength.
Your physiotherapist will design an individualised exercise programme that will include neck stretches, dynamic strengthening, and core strengthening and stability work. These exercises will not only focus on your neck, but also target your upper back, shoulders and arms. This will give you maximum strength and stability throughout your spine and upper body.
Having regained a good range of movement and level of muscle strength, functional training helps you resume more demanding activities. Everyone has different demands for their bodies that determine what specific treatment goals they want to achieve;
depending on your occupation, or chosen sport or hobby, your physiotherapist will tailor your rehabilitation to work on functional and activity specific movements or tasks, to allow you to return to your desired activities safely.
Posture Re-education
In order to help prevent worsening or recurrence of symptoms your physiotherapist will work on your posture and correct any abnormal movement patterns.
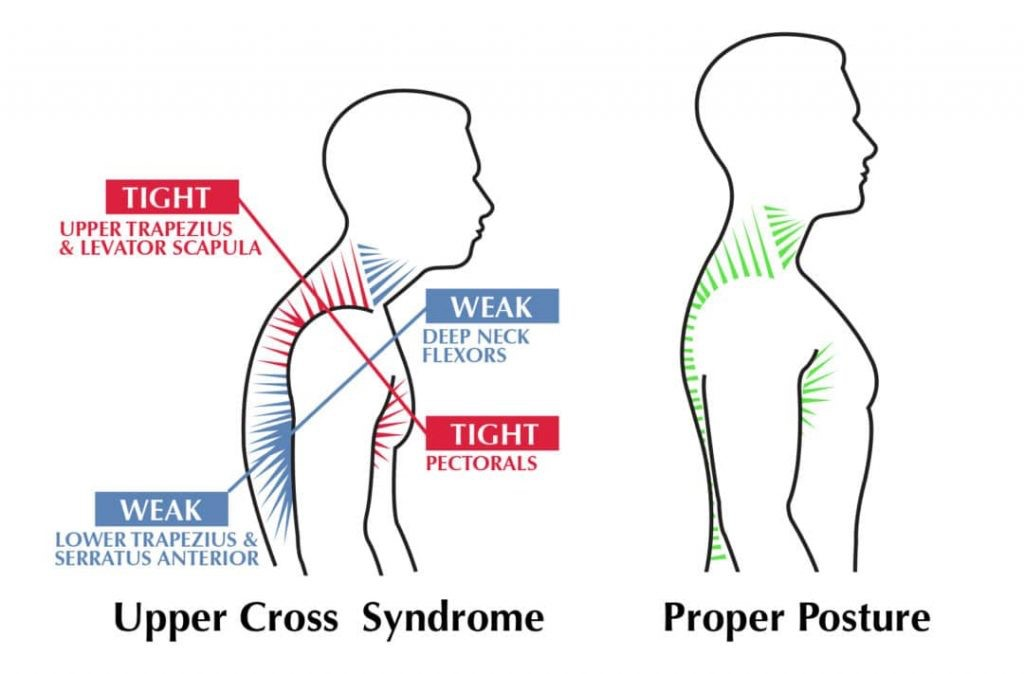
If you spend long periods sitting at your desk/computer, you will also benefit from having an ergonomic assessment to look at your work space and your posture, and give you tips on how to reduce further flare ups.
Your physiotherapist may also suggest that you commence a course of Pilates, which is a highly effective way of managing more chronic cervical spine pain and radiculopathy and can vastly improve your movement and posture. Complete Pilates offers a variety of 1:1 and group classes.

At Complete Physio we are experts in the treatment and management of cervical radiculopathy; we are dedicated to getting our patients out of pain and back to full function.
We have clinics across London, and can often offer urgent, same day appointments if required.
Cervical Spinal Injections for Radiculopathy
If other treatments do not significantly relieve your pain and symptoms, a cervical epidural steroid injection might be a treatment option for you.
We do not carry out this treatment at Complete Physiotherapy, however we have excellent links to some of the best spinal and pain medicine specialists who we can refer you directly to.
A cervical epidural steroid injection is a minimally invasive procedure that involves injecting a combination of numbing medication (anaesthetic) and corticosteroid (also known as steroid or cortisone) into the epidural space around the spinal nerves.
Cortisone is a very strong anti-inflammatory medicine; by injecting this near the pinched nerve it can reduce swelling and relieve pain.
Although the injection won’t relieve the pressure on the nerve caused by a narrow foramen or by a bulging disk; by reducing the swelling and giving the nerve some time to heal, it will allow you a window of opportunity to engage fully in your Physiotherapy programme.
Once your pain has settled from the injection (approx 1 week), you should re commence your rehabilitation under the guidance of your Physiotherapist at Complete. Injections should never be used as a stand alone treatment.
The pain relief can last from a few weeks to years and if you experience a recurrence of pain, the procedure can be repeated.
Your Physiotherapist can refer you to a spine or pain consultant who can administer these injections.
Spinal Surgery for Cervical Radiculopathy
In some cases, cervical radiculopathy does not improve with non surgical intervention. If this is the situation then you may require surgery. This is only usually advised if you have tried all other conservative options and you still show signs of:
- Unbearable pain
- Increasing upper limb weakness
- Increasing numbness
- Muscle wasting
- Disruption to normal daily life and function
- Deteriorating mental health due to ongoing pain
One of the most common operations used to treat cervical radiculopathy caused by pressure from bone spurs or a herniated disc is the Anterior Cervical Fusion. Other surgical options include an Artificial Disk Replacement (ADR) or a Posterior Cervical Laminoforaminotomy. Your surgeon will discuss all your options with you, and make sure they choose a procedure that is best for you.
After surgery you will need to recommence your Physiotherapy treatment. We work very closely with your surgeon to ensure that all post-op protocols are followed, and that we optimise your surgery outcome.
Regardless of whether you require a conservative or surgical approach, we will be there to support your recovery every step of the way.
If you would like to book an appointment or speak to one of our expert physiotherapists please call 020 7482 3875 or email info@complete-physio.co.uk.
Don’t let pain hold you back, book now!





