
What Is Hamstring Tendinopathy?
Proximal Hamstring Tendinopathy (PHT), also known as high hamstring tendinopathy, is inflammation in the tendons at the back of your thigh. It typically manifests as deep buttock pain at the top of the hamstring – where it attaches onto the sit bone of your pelvis. It is very common in runners and can be a very stubborn condition to get better. At Complete Physio, we treat hundreds of proximal hamstring issues every year and so have the experience and knowledge to get you out of pain and back to full function.
Hamstring tendinopathy occurs when the tendon is overused or overloaded. The process can occur over many weeks or months, or can happen more rapidly with one, highly intense exercise/activity. It tends to be aggravated by activities such as hill climbing, dancing, cycling or long distance running, but it can also be caused by prolonged compression from sitting or driving.
If not treated properly, it can be a persistent and recurring problem.
Anatomy of the Hamstrings tendons
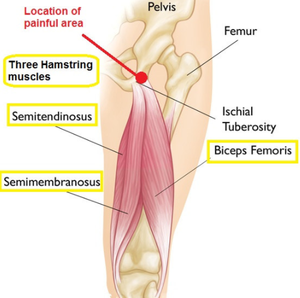
The Hamstrings are a large, powerful muscle group that is made up of 3 muscles (semimembranosus, Semiteninosus, Biceps Femoris), which attach from the bony prominence in the buttock (Ischial Tuberosity), to behind the knee (Tibia and Fibula) and thigh bone (Femur). The Hamstrings work to bend the knee and extend your leg back behind you, but most importantly, they also function to control and slow down knee straightening.
Tendons are fibrous cords, and are made of collagen; you can imagine the structure of the tendon looking like ‘rope’. They have a blood supply, which helps them to repair when damaged. Tendons attach the muscles to bone. As the muscle contracts it pulls on the tendon, and the tendon moves the bone to which it is attached, as well as any joints it crosses. This is how your joints and limbs move.
The issue with tendon issues is they have a relatively poor blood supply compared with muscles for example. This means that although they do heal, they are often slow to heal. Patients and perseverance of often required with tendon complaints.
What causes Hamstring Tendinopathy?
The exact cause is unknown but research suggests that it is related to repetitive strain, and overload of the tendon.
Tendons are designed to withstand high, repetitive loading; however when the hamstring tendon is subjected to excessive, high-intensity activity, it sustains small micro-tears, which causes inflammatory chemicals and swelling (tendonitis). This mild trauma quickly heals if managed appropriately with rest and a reduction of high impact forces. This phase is known as the Reactive Stage.
However, when the tendon is subjected to continuous, repetitive forces it causes increased micro-injury. This ongoing trauma occurring in the tendon can exceed the rate of repair, resulting in disruption of the tendon fibres and an incomplete, sub-optimal healing response. This is called the Degenerative Stage.
Damage can progressively become worse over time, causing the tendon to become even more inflamed and thickened. This results in significant pain and dysfunction, and in severe cases can result in larger tears or even tendon rupture.
The Hamstrings are prone to this type of overuse injury as they control the slowing down of a straight knee during activities such as long distance running, sprinting, hill climbing/running or kicking. This is because the deceleration forces from these activities, places excessive, constant strain on the tendon.
In some cases, pain can be elicited with the compressive force on the hamstring insertion from sitting for long periods of time.
Common Causes:
- Compressive loads – Running, prolonged driving or sitting
- Uphill or downhill running
- Deep lunges or squats with excessive load
- High speed running
- Long distance running
- Long distance cycling
- Kicking a football or rugby ball
Intrinsic Risk Factors:
- Previous hamstring injury
- Gluteal or Hamstring muscle weakness
- Obesity – increased BMI can cause added strain on your muscles, joints and soft tissues.
- Age – Over 40 – As people age, their muscles and tendons can lose some strength and elasticity, which may increase chances of hamstring tendinopathy.
- Core muscle weakness
- Hip joint stiffness
Extrinsic Risk Factors:
- Training changes – A sudden change in intensity or frequency.
- Inadequate rest between training sessions – Causing tendon overload
- Inadequate equipment – Incorrect size of bike, poor fitting or worn out trainers.
- Insufficient warming up and cool down
- Fatigue – Injury risk can significantly increase when the body is tired.
- Poor Technique – Such as overstriding when running.
What are the Symptoms of Hamstring Tendinopathy?
The main symptom is a dull, deep pain, or aching, in your buttock. The pain often extends down into the hamstring muscle.
Symptoms usually present gradually, without trauma, over a few weeks or months of repetitive overloading.
When you first feel pain, it will likely come on a short time after you exercise, and will settle down by the evening. But as time goes on you may start to feel pain during and after exercise. This can then develop into constant pain even with normal daily activities.
Sometimes symptoms can also come on more quickly if you have suddenly upped your training/activity level in a short space of time, or done a one off event without adequate training.
Symptoms of hamstring tendonitis may include:
- Dull ache in your buttocks, the back of your thigh, knee or lower leg
- Leg stiffness when walking or bending your knee.
- Pain made worse with stretching or exercising the hamstring.
- Weakness in the hamstring muscles at the back of your thigh.
- Pain with running, lunging or squatting.
- Pain when sitting, especially on a hard surface.
How do we Treat Hamstring tendinopathy?
Most people with hamstring tendinopathy pain respond very well to conservative management strategies. This will include a progressive, loading exercise programme, designed and managed by your Physiotherapist; as well as other treatment modalities such as manual soft tissue techniques, shockwave and functional/sports specific rehabilitation.
It is however important to be aware that tendon complaints can sometimes be slow to improve, and often take several months to resolve; especially if you’ve had the problem for a number of months. Rehabilitation takes both patience and persistence.
Complete Physio has an excellent reputation for providing a first class, highly specialised tendon rehab clinic. We treat everyone, from elite athletes and Professional footballers, to recreational cyclists and Park Runners, but also the older population who lead a less active lifestyle. Some of the most experienced and world renowned Orthopaedic Surgeons and Sports Medicine consultants refer their patients to us.
Physiotherapy and Rehabilitation
Rest and Activity Modification
The good news is you rarely have to completely rest from all sports and activities. Your Physiotherapist will give you advice on how to modify your training programme to ensure that you optimise recovery, and also maintain your fitness.
Activities such as sprinting, long distance running, hockey, rowing, or uphill running are more provocative. It will be sensible to limit these activities to shorter sessions per week, and allow sufficient recovery time between sessions. Cross training is recommended to improve fitness without further irritating the hamstring tendon. This may include using a static bike, swimming or using an elliptical machine.
If compression aggravates your symptoms you may also need to modify your work space so that you perch or stand at your desk, rather than sitting for long periods.
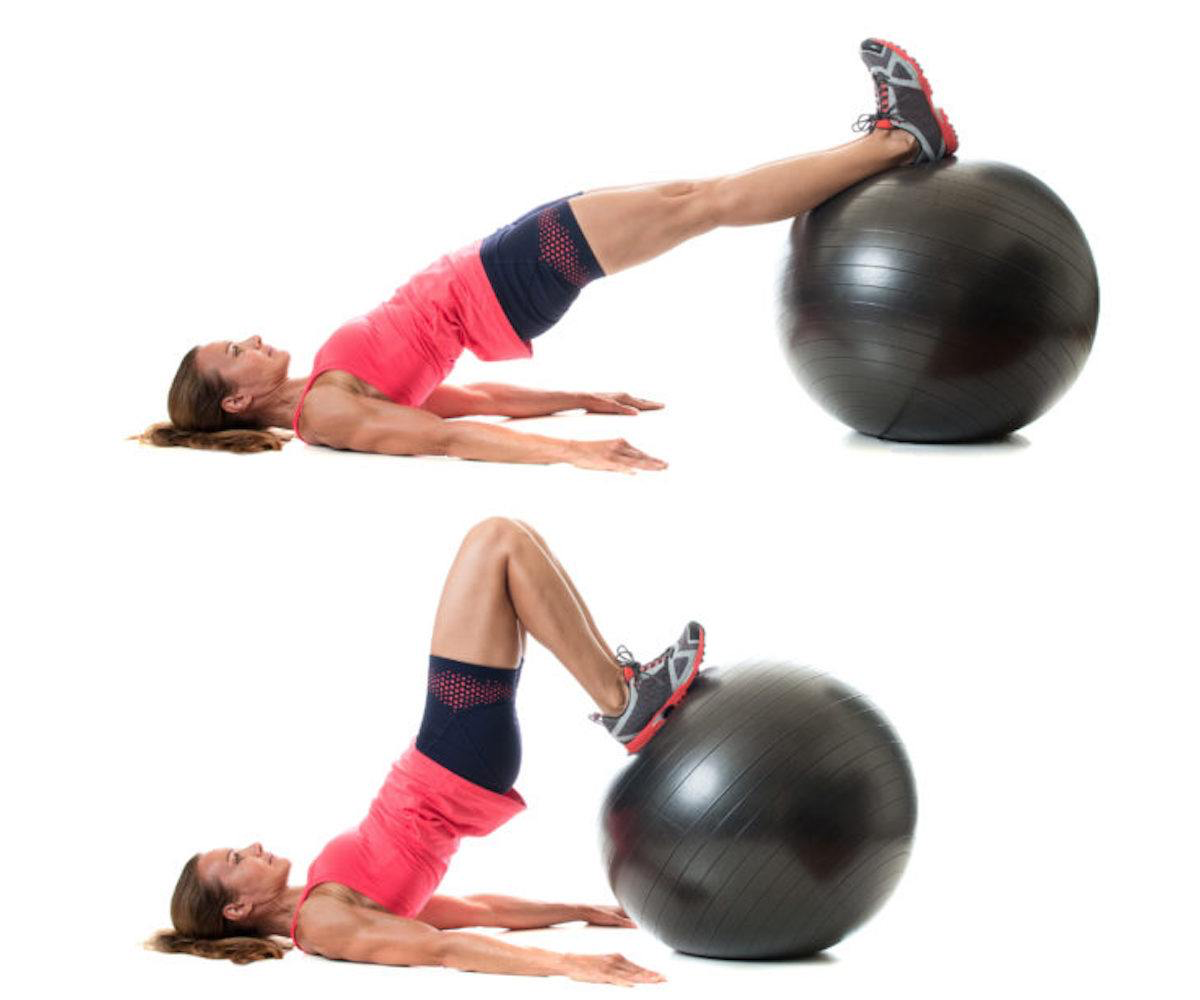
Strengthening Exercises
Heavy, slow resistance (HSR) training for your hamstring muscles, has been shown to have the best stimulus for improving tendon structure and repair.

Strengthening exercises for the muscles that support the hamstring, such as the gluteal (buttock) muscles, adductors, calves and quads are also an essential part of treatment. When the supporting muscles are weak, especially the glut’s, the hamstrings have to work much harder. By improving the strength of these supporting muscles it reduces the forces going directly through the hamstring muscle and tendon and therefore protects it.
A lower limb strengthening programme will be put together by your physiotherapist, based on your clinical assessment and goals. It is important to be committed and consistent with your exercises in order to maximise your recovery.
Exercise and Activity Load
Appropriate exercise load and intensity management is vital to the successful treatment of proximal hamstring tendinopathy. Mild and gradual load increases will stimulate new tendon growth, whereas overload leads to further tendon deterioration.
Tendons are known to have a latent response to loading, which means they can take 24 hours or more to react and become sore. When managing activity and rehab exercises, it’s important to be guided by how the tendon responds immediately and up to 24 hours later.
Getting the balance right is critical, which is why it is important to work closely with an experienced Physiotherapist, who will guide your progression.
Other treatments may include:
- Over-the-counter nonsteroidal anti-inflammatories and painkillers – To help manage your pain and allow you to carry out daily activities without excessive discomfort.
- This should always be discussed with a GP or pharmacist.
- Ice therapy – This can be applied for at home two or three times throughout the day to help with pain and inflammation.
- Range-of-movement exercise – Your physiotherapist may teach you self-stretching methods. These can decrease tension and help restore normal motion of your injured joints. It is important not to over stretch when you have a hamstring tendinopathy, therefore you will need to be guided by your therapist.
- Manual therapy – In order to help improve movement and reduce muscle stiffness your physiotherapist may use manual therapy such as massage or soft tissue release techniques to the surrounding muscles.

- Movement re-education – This may involve teaching you how to correctly squat, lunge, run or jump. For those who need more in depth assessments Complete have a specialised running and cycling clinic available to our patients.
- Acupuncture – may be used to help your pain and encourage more blood flow to the region. It can also be used to help tight regions in the hamstring muscles.
- Functional and sports specific training – once your pain, strength, and range of movement improve, functional training can help you safely resume more demanding activities and get you back to playing the sport that you love.

If, after a number of more traditional physiotherapy treatments, your symptoms are not settling and resolving, there are a few further treatment options available.
- Shockwave therapy
- Ultrasound guided injection
1) Shockwave Therapy – also known as Extracorporeal Shockwave Therapy (ESWT)
Shockwave therapy is an evidence-based treatment modality used in sports medicine for treating tendon pain. This treatment works in two ways; firstly, it is designed to deliver a series of powerful sound waves which causes controlled micro-trauma to the affected tendon. This initiates your body’s natural healing process. Additionally, shockwave treatment desensitises local nerve endings around the tendon, causing a reduction in pain. This can provide a window of opportunity to progress with your rehabilitation regime.
Recent evidence suggests optimal outcomes for the treatment of lower limb tendinopathies, following 3-5 shockwave treatment sessions, running concurrently with a progressive physiotherapy led exercise program.
Shockwave therapy is available at three of our Complete clinics – Bury Street (next to Gherkin), Chelsea and Angel clinics.
-
Ultrasound guided injections
Injection therapy is used within Musculoskeletal Medicine to reduce pain and inflammation, allowing you to progress your physiotherapy treatment and more effectively rehabilitate your condition.
Steroid Injections
If symptoms continue, it may be that an ultrasound guided steroid injection would be appropriate for you. Steroid is a strong anti-inflammatory and is used for many tendon complaints, and will help relieve inflammation and pain
We combine a small amount of local anaesthetic with the steroid to reduce any pain associated with the procedure. You should expect you to get rapid pain relief 3-4 days following the injection. We always encourage you to restart your rehabilitation exercise as soon as your pain has reduced.
Platelet Rich Plasma (PRP) Injection
Another type of injection therapy available at Complete is ultrasound-guided platelet-rich plasma (PRP) injection.
We combine a small amount of local anaesthetic with the steroid to reduce any pain associated with the procedure. You should expect you to get rapid pain relief 3-4 days following the injection. We always encourage you to restart your rehabilitation exercise as soon as your pain has reduced.
Platelet Rich Plasma (PRP) Injection
Another type of injection therapy available at Complete is ultrasound-guided platelet-rich plasma (PRP) injection.
PRP has been clinically proven to enrich the healing process and speed up the recovery of tendons. It is a natural, safe treatment for Hamstring Tendinopathy which uses components of your own blood, which is injected in and around the hamstring tendon, to promote healing. There are very few side effects and the procedure is well tolerated, however it is reserved for cases that have failed to respond to all other treatment options.
Research suggests that a series of three injections is required to successfully treat tendinopathic pain.
Will I Need Surgery For Proximal Hamstring Tendinopathy?
Very few people require surgery for hamstring tendinopathy. If you have a severe tendon tear, or the tendon tears away completely from the bone (avulsion), you might need surgical treatment to repair this.
To repair a tendon avulsion, your surgeon must pull the hamstring tendon back into place and then reattach the tendon to the bone using small devices called anchors.
Rehabilitation following a proximal hamstring reattachment typically starts a week or two after surgery and can take at least 6 months, due to the severity of the injury.
At Complete Physio, we work with some of the most experienced and highly qualified Orthopaedic Surgeons in the country, we will ensure that you get the best care possible, and will take you through your post op rehabilitation step by step, to get you back to pre-injury fitness.
If you would like to book an appointment to see one of our expert physiotherapists please call 020 7482 3875 or email info@complete-physio.co.uk.
Don’t let pain hold you back, book now!




