What is Greater Trochanteric Pain Syndrome – GTPS (also known as “Trochanteric Bursitis”)
GTPS or trochanteric bursitis is a common condition which is characterised by persistent pain along the outer side of your hip, buttock and thigh. This is usually caused by an injury or irritation to the soft tissue structures (muscles, tendons, bursa) that lie over the top of your outer thigh bone.
It classically causes pain with walking particularly upstairs, lying on your side at night and running.
It is more common in women over 40’s and the prevalence increases with age. It can also be related to other conditions such as osteoarthritis of the back and hip and femoral acetabular impingement (FAI).
Anatomy of the hip
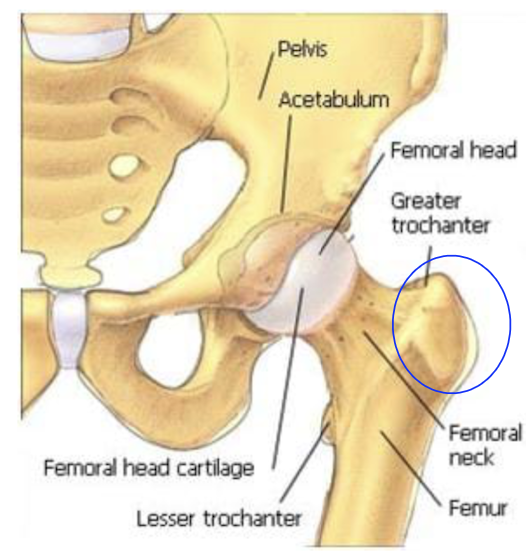
The greater trochanter is the large bony protuberance on the side of your hip located at the top of the thigh bone. This bone is the attachment site for your gluteal muscles (gluteus medius and gluteus minimus); these are two of the bum muscles that help move and stabilise your hip. They start from your pelvic bone and then join to form a tendon, which attaches onto the greater trochanter of your thigh bone. This tendon is an area that can become damaged through injury or overuse.
You also have a tough band of connective tissue called your ITB. This tissue can also contribute to symptoms of GTPS. If it becomes tight, it can compress and irritate the trochanteric bursa.
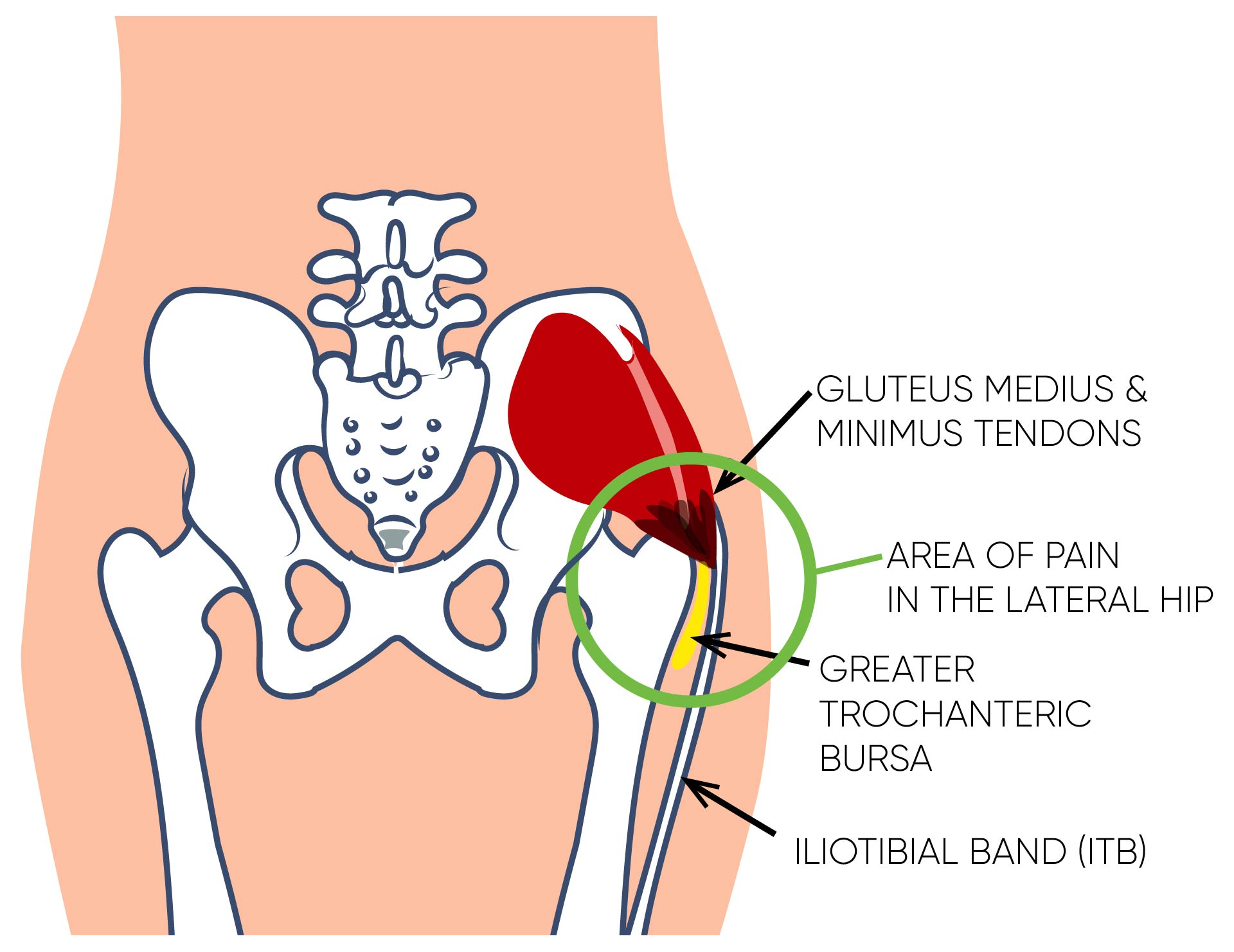
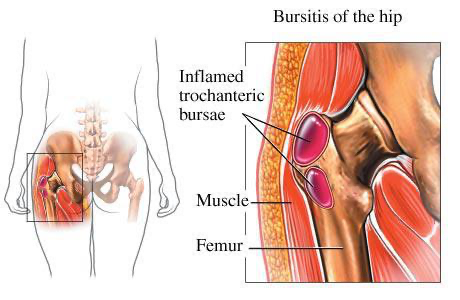
The trochanteric bursae are potential spaces between two anatomical structures. The bursa is located between the bony prominence of the femur, called the greater trochanter, and the soft tissues (muscles,tendons and ligaments) on the outside of the hip. The role of the bursae is to help reduce friction and ensure there is smooth movement between the bones and the soft tissues. They also act as a protective pad which reduces the risk of injury from direct impact. There are several bursae that can be associated with GTPS, most commonly it is the trochanteric bursa. If the bursa becomes inflamed and swollen i.e. there is excessive fluid in the bursa, it becomes known as trochanteric bursitis.
What are the causes of Greater Trochanteric Pain Syndrome (also known as Trochanteric Bursitis)?
GTPS was traditionally known as trochanteric bursitis as it was thought that the pain was purely linked to the trochanteric bursa. Research has now shown that pain is often generated by not just the bursa but also a number of soft tissue structures around the outside of the hip; namely the muscles and tendons. Therefore, in the medical literature, the term Greater Trochanteric Pain Syndrome (GTPS) is now more commonly used, as it reflects the different structures that can be involved. These include gluteus minimus or medius tendinopathy, or tears of the gluteus medius or minimus tendons/muscles.
The management strategies and treatment can vary significantly depending on which of these specific structures are affected. It is therefore vital to have a full assessment by an expert physiotherapist to ensure you engage in the correct treatment programme. On occasions a diagnostic ultrasound scan is required to identify exactly which structures are involved.
Tendinopathy
One of the primary causes of Greater Trochanteric Pain Syndrome (GTPS) is thought to be tendinopathy of the gluteus medius and minimus muscles.
Tendinopathy is associated with a failed healing response to an overuse injury or sudden stress on the tendon (microtrauma). The tendon becomes swollen and sore, and overtime becomes thickened; this process is known as tendinopathy.
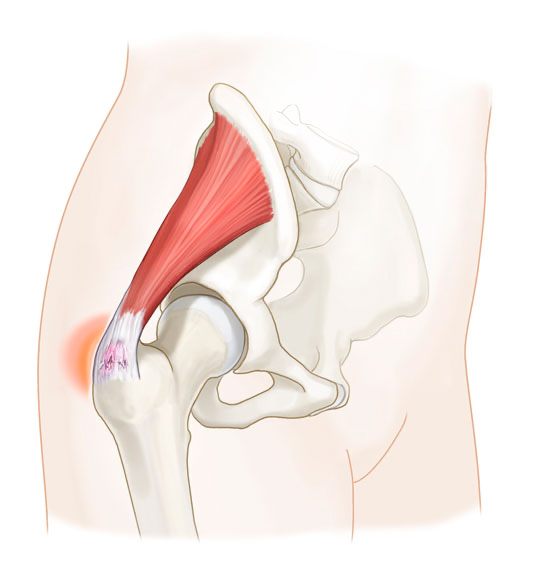
The image represents inflammation of the gluteus medius tendon as it attaches onto the greater trochanter pain. This can cause pain on the outside of the hip.
Bursitis
Bursitis is a condition whereby the bursa membrane becomes inflamed due to one or more of the below risk-factors, and causes excess synovial fluid to be produced, making the bursa swell and fill with fluid. This swelling and inflammation results in pain.
Causes of GTPS include:
- Direct Injury/Impact – Direct trauma to your lateral hip, such as a fall on a hard surface, onto the side of your hip.
- Excessive, Repetitive Movements (overuse) – This can occur when running, stair climbing, cycling, or standing for long periods of time, especially if you have not gradually increased your training.
- Prolonged or Excessive Pressure – This compression injury can be sustained from sleeping on a hard surface while camping or from prolonged sitting in a low chair, or from crossing your legs for an extensive period.
- Bone Spurs/calcification – These are extra areas of bone growth that can develop on the bone or within the tendons that attach your gluteal muscles to the greater trochanter. They can irritate the tendons and the bursa and cause inflammation.
Risk Factors
- 4 times as many women get GTPS than men
- Most common in people aged between 40-60 years old – although it can affect people of any age.
- People with chronic lower back pain will often also develop GTPS.
- Medical conditions such as Osteoarthritis, Rheumatoid Arthritis, Diabetes and Gout can all make someone more prone to GTPS.
- Increased BMI – People who are overweight tend to be more affected.
- Tight hip muscles and Iliotibial band (ITB)
- Sedentary lifestyle i.e. lack of regular exercise
- Hip muscle weakness – particularly weakness of the gluteal muscles and core stability muscles. These weaknesses result in poor hip and pelvic stability and control, causing increased pressure on the soft tissue structures around the hip, making them more susceptible to injury.
- Different leg lengths and pelvic asymmetry – many of us have one leg longer than the other. But if this is significant (>1cm), this can alter the body’s biomechanics when walking and running, and can again cause added stress on the structures around the hip. There are two reasons why you can have a long leg on one side; 1/ You actually have a longer bone on one side, this is known as a “true” leg length discrepancy or 2/ your pelvis is rotated (“twisted”) on one side and this causes an “apparent” leg length discrepancy. The second reason can be corrected with physiotherapy. A thorough physiotherapy assessment will be able to identify if you have a “true” or “apparent” leg length discrepancy.
- Poor technique – If your running gait or cycling technique is not correct, this can alter the way that your pelvis and lower legs move, putting pressure and stress through the muscles and joints.
- Inadequate training – This is commonly observed in runners and cyclists, who increase their training too quickly.
What are the symptoms of Greater Trochanteric Pain Syndrome (also known as Trochanteric Bursitis)?
Greater Trochanteric Pain Syndrome or trochanteric bursitis, typically begins gradually over a few weeks or months. Symptoms often begin as intermittent episodes of pain which resolve with a short period of rest. These episodes become more frequent and last longer, giving little relief of symptoms in between.
On occasion, the pain can start suddenly due to a specific injury, or because of a very sudden increase in activity over a short period of time.
The condition causes pain on the side of the hip, that can radiate into the buttock region and down the leg.
Specific symptoms can vary from person to person depending on the factors that are causing or contributing to the condition. People may experience:
- Pain in the outer bottom/thigh/buttock area.
- Worse pain when lying on your side – the pain often disturbs sleep and is worse at night.
- Increased pain with exercise, such as long periods of walking, standing, cycling or running.
- Altered walking pattern – due to pain and/or weakness.
- Tenderness to touch on the outside for your hip bone. This may also be associated with swelling.
- Pain sitting with your legs crossed.
- Walking up slopes or upstairs may make the pain worse.
- Stiffness after prolonged sitting – especially in a low chair.
If any of these symptoms describe what you are feeling, and you would like to speak to one of our team, or book in to see a physiotherapist, then please get in touch by calling 0207 482 3875 or by emailing info@complete-physio.co.uk.
How is Greater Greater Trochanteric Pain Syndrome (also known as Trochanteric Bursitis) diagnosed?
Your physiotherapist will use a combination of medical interview, clinical tests and diagnostic imaging to confirm your diagnosis. It is vital that you get an accurate diagnosis of the condition and also the underlying cause, in order to ensure that you are started on the most appropriate treatment.
At your initial appointment your physiotherapist will ask questions about your past health, symptoms, aggravating and easing factors, activities and exercise regime. This will help to build up a picture of what is likely to be causing the problem.
After your consultation, your specialist physio will complete a series of clinical tests to confirm their diagnosis; this may include:
- Assessing the range of movement of your hip joint, and the strength of your lower leg muscles.
- Assessing muscle length and flexibility of lower leg muscles – especially the gluteal muscles and the hip flexors.
- Assessing your leg length and pelvic symmetry.
- Watching you move your hip and how you perform activities such as squatting, hopping, jumping, running.
- Checking other regions of the body as needed; such as lower back, knees and feet. This will help to determine if other areas are contributing to the problem, and also require treatment to improve your condition. Just because your pain is in one region does not mean that that region is the cause of the pain or even the structure causing the pain.
- “Referred pain” is a type of pain that is felt in a part of the body that is different from the source of the pain. It can occur due to the overlap of pain pathways in the nervous system.
- Gently, but skilfully, feel around your hip and pelvis to find exactly where it is most painful and to assess for any restriction in joints and muscles.
While a clinical assessment is normally sufficient to diagnose GTPS, it may not give you details of the exact structure causing the pain and further investigation/imaging may be required. We would certainly suggest further imaging is appropriate if your pain is not improving.
What is the best imaging for Greater Trochanteric Pain Syndrome or trochanteric bursitis?
This will depend on your initial assessment. They will consider history, onset of symptoms and location of pain. The most appropriate imaging technique will depend on your specific presentation. Be aware there are many other conditions that can mimic the pain associated with GTPS and trochanteric bursitis, the most common are:
- “Referred pain” from the lower back and/or sacroiliac joints (SIJ).
- Femoral acetabular impingement (FAI)
- Hip osteoarthritis
- Proximal hamstring tendinopathy
- Stress fracture of the femur (specifically the femoral neck)
Diagnostic Ultrasound
For a majority of suspected GTPS and trochanteric bursitis that are not improving, a diagnostic ultrasound scan is an appropriate first imaging technique. Diagnostic musculoskeletal ultrasound imaging is normally reserved for those who are unsure of their diagnosis, are concerned that the tendon may have significant tear and/or the pain is not improving as we would expect.
Diagnostic ultrasound has been proven to be an effective diagnostic tool for the evaluation of the gluteal tendons and bursae. Ultrasound is as sensitive as an MRI scan to confirm a bursitis and or a tendinopathy or tendon tear. Ultrasound produces real-time, dynamic images that are capable of not only evaluating tendon structure but also inflammation and swelling associated with both tendinopathy and bursitis. Diagnostic ultrasound can also be used to carry out an ultrasound guided steroid injection into the trochanteric bursitis if appropriate. This often provides fast acting pain relief.
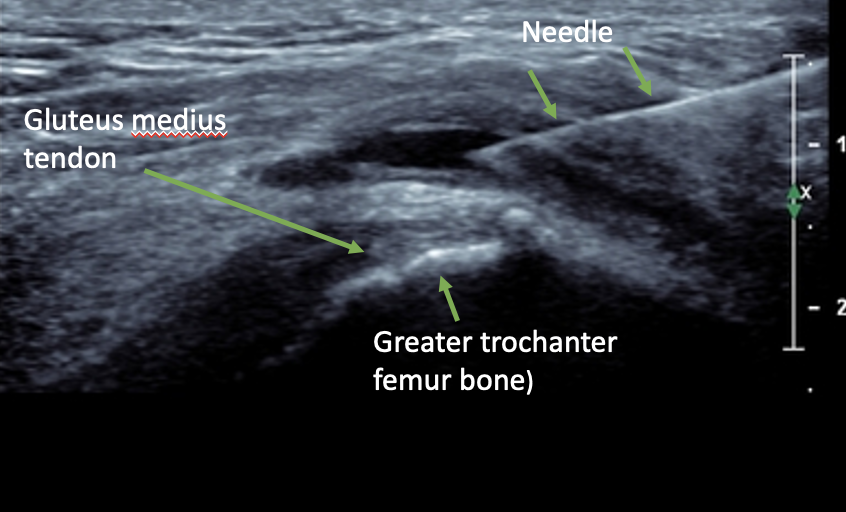
Ultrasound image of the hip tendons and trochanteric bursa
Complete Physio leads the way within the private sector, as we are able to offer diagnostic ultrasound imaging as part of our assessments, at no extra cost, and without having a GP referral. If you think that you will need a scan, you must be booked in to see one of our Clinical Specialists, who are specialist physiotherapists and trained musculoskeletal sonographers. Our Clinical Specialists, also carry out a variety of ultrasound guided injections following the ultrasound scan if deemed an appropriate next step. Please inform our booking team at the time of making your appointment if this is a service you require.
MRI
An MRI scan is not required for diagnosing GTPS. MRI is a static test that can visualise the deeper structures in the hip joint better than ultrasound, such as the articular cartilage on the joint surfaces or the labrum of the hip. MRI is also excellent at diagnosing stress fractures, and issues with the lower back (lumbar spine) and sacroiliac joints (SIJ).
X-Ray
An X-ray is not able to diagnose GTPS as the tendons and bursae will not show up on x-ray, however it can be used to rule out any bony abnormalities like bone spurs, or damage to the joints such as osteoarthritis. It can also visualise some stress fractures, but not all of them. MRI is better for stress fractures.
How do we treat Greater Trochanteric Pain Syndrome (also known as Trochanteric Bursitis)?
Over 90% of people with greater trochanteric pain syndrome recover fully with conservative treatment such as rest, pain relief, physiotherapy, or corticosteroid injection.
Physiotherapy and Rehabilitation
At Complete Physio we are highly experienced in treating GTPS, and your physiotherapist will take you through a specific, tailored rehabilitation programme based on the findings from your clinical assessment.
Physiotherapy often comprises of 4 different aspects
- Education and patient engagement.
- Pain relief, rest and activity modification.
- Regaining normal movement, flexibility and strength.
- Restoring full function and resuming normal activities/sport.
Patient Education
- It’s important to understand your condition and to take an active part in your recovery. We will ensure you are given a clear explanation of the diagnosis and any other underlying causes, and we will discuss what is required to optimise your recovery and reach your treatment goals.
Rest and Pain Relief
- You will be given advice on relative rest and how to modify your activity or training in order to give your pain and symptoms a chance to settle, and for your body to begin to heal.
- Ice can be a good way to help manage pain and swelling – this can be done at home.
- Painkillers and anti-inflammatory medication are useful in the early stages of management. Especially if your pain is disrupting your sleep and preventing you from performing your normal daily activities. (any medication needs to be approved by a pharmacist or doctor)
- Acupuncture – Your therapist may suggest a few sessions of acupuncture to help reduce pain and stimulate tissue healing.
- Shockwave – Shockwave therapy or extracorporeal shockwave therapy (ESWT) is an innovative, evidence-based treatment for tendon pain, and can be used to treat gluteal tendinopathy (more later about shockwave)
Movement, Flexibility and Strength
Once your pain is starting to settle, you will begin an exercise programme to regain full range of motion and muscle strength. This will be specific to your individual needs and rehab goals.
- Your physiotherapist may teach you self-stretching methods. These can decrease tension and help restore normal movement of your injured muscles and joints.
- Hands-on massage and joint mobilisations can be a good way to loosen up the soft tissue and stiff joints around the pelvis and lower back.
- Strength and loading exercises – Your physiotherapist will design a safe resistance program to ensure all your muscle groups, especially your glutes, are strong and working in synergy. You will be given exercises to continue independently; this is a key component of your treatment programme and will require some commitment and consistency.
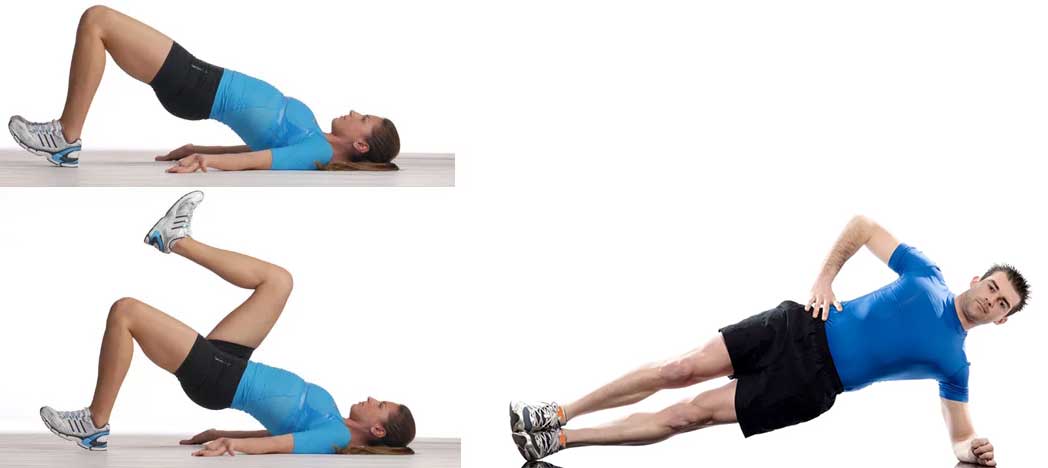
- Pilates – This is a fantastic way to develop pelvic and core stability which is a vital part of your recovery process. Complete has a specialist team of physiotherapists and pilates instructors who can offer this as part of your treatment, or as part of a longer term conditioning programme.
Functional and sports specific training
The final stage of your rehabilitation aims at returning you to your desired activities. Everyone has different demands for their hip; for some people it may be only to walk around the block, others may wish to run a marathon. Your physiotherapist will tailor your hip rehabilitation to help you achieve your own functional goals and help you safely resume more demanding activities and sports.
As part of your assessment and treatment, your Physiotherapist may want to analyse your walking and running style, to work on correcting your technique and to help you move more efficiently. Complete Physio also offers a full running assessment service for patients who have very specific running goals.
What if your GTPS (trochanteric bursitis) is not improving?
If your GTPS is not improving with physiotherapy alone there are two main treatment options:
Shockwave Therapy
Shockwave therapy or extracorporeal shockwave therapy (ESWT) is an innovative, non-invasive evidence-based treatment for tendon pain, and can be used to treat gluteal tendons. Shockwave therapy uses high-energy sound waves to stimulate the healing process in damaged tissues. It has been used to treat a variety of musculoskeletal conditions, including GTPS.
In the case of GTPS, shockwave therapy is thought to stimulate the production of collagen, which can help to strengthen and repair damaged tissue in the hip region. It may also help to reduce inflammation and improve blood flow to the affected area. Shockwave therapy is generally considered a safe and effective treatment option for GTPS, and most people experience significant pain relief after just a few sessions.
Follow this link for more information on shockwave therapy for GTPS.
Ultrasound Guided injections
Greater trochanteric pain syndrome normally responds well to a course of physiotherapy and/or shockwave therapy. However, if the pain and other symptoms are not improving, or your sleep and daily activities are being significantly affected, then ultrasound guided injection therapy can provide rapid pain relief. After an injection we would always recommend a course of physiotherapy to continue to treat the root cause of your symptoms and ensure the pain does not return.
There were two clinically effective, evidence-based injection options that Complete offer, for the treatment of GTPS. Both are carried out with ultrasound guidance.
These techniques are corticosteroid injection and platelet-rich plasma (PRP) injections.
A Corticosteroid injection is carried out using ultrasound guidance into the trochanteric bursa. Corticosteroid, also known as cortisone, is a strong anti-inflammatory medication which reduces the inflammation and consequently your pain. Improvements in pain are normally felt within a week. At Complete all our injections are carried out using ultrasound guidance to ensure the accuracy and effectiveness of the injection. For more information about our ultrasound guided injection service click here.
Platelet-rich plasma (PRP) injections is a novel, natural injection which does not use drugs. Platelet-rich plasma (PRP) injections are a type of treatment that involves injecting a concentrated solution of platelets from your own blood into the injured area of the body. Platelets are a type of blood cell that play a crucial role in the healing process. They contain growth factors and other proteins that help to stimulate the production of new tissue and promote healing.
To prepare the PRP solution, a small sample of the patient’s blood is drawn and then placed in a centrifuge to separate the platelets from the other blood cells. The concentrated platelet solution is then injected into the injured area. The injection process typically takes just a few minutes, and most people experience little to no discomfort during the procedure.
Both injections should be followed up with a course of physiotherapy.
For more information about our ultrasound guided injection service click here.
Greater Trochanteric Pain Syndrome Surgery
Surgery is very rarely required or performed, however, in persistent cases, removing the bursa – known as a bursectomy, can be performed. Or if your symptoms are being caused by issues with the tendons and soft tissues, then these can be released to reduce the pressure and friction.
If an onward referral is required we will ensure that you are provided with exceptional care from one of the highly experienced, Orthopaedic Consultants who we work closely with. Following your surgery you will require physio rehabilitation, and so we will ensure that we continue to support your post-op recovery every step of the way.
Don’t let pain hold you back, book now!






