1. What is GTPS?
GTPS is a common cause for pain on the side of the hip (see image below). The hip joint is made up of a ‘ball and socket’. The ‘ball’ is the head of the thigh bone (femur) and the ‘socket’ is your pelvis (also known as your acetabulum). The greater trochanter (GT) is the bony protuberance on the side of your hip located on the thigh bone. This bone is the attachment site for tendons namely your gluteus medius and gluteus minimus. Above the tendons is a thin fluid filled layer called the bursa and the iliotibial band (ITB), which is attached to the tensor fascia latae (TFL). The role of the bursa is to prevent friction of the tendon’s as they move over the bone with hip movements and the role of the ITB and TFL is to move and stabilise the hip and pelvis.
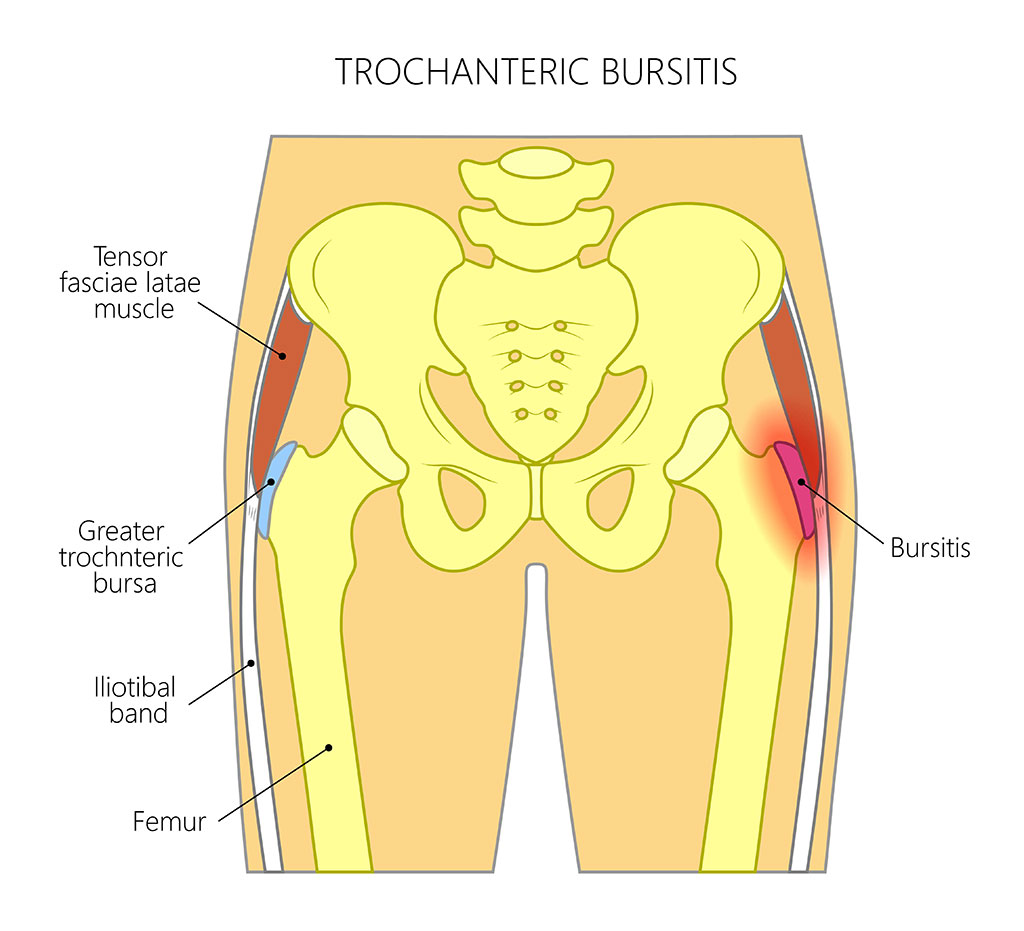
Historically, it was suggested that the pain was linked to inflammation of the trochanteric bursa. However, this rather simplistic explanation has been disputed and the condition is now being referred to as greater trochanteric pain syndrome (GTPS). This term encompasses numerous structures around the outside of the hip, the gluteal tendons specifically the gluteus medius tendon (Barratt et al., 2017; Carlisi et al., 2019). It is now considered that the pain is generated from both the tendons and the bursa. At Complete we believe it is essential to consider both of these structures in the treatment plan.
The condition causes pain on the side of the hip that can radiate into the buttock region and down the leg. GTPS does not normally limit or cause pain when taking off shoes and socks. Pain on removing shoes and socks is more associated with hip joint issues such as osteoarthritis or femoral acetabular impingement (FAI) (Twin et al., 2014)
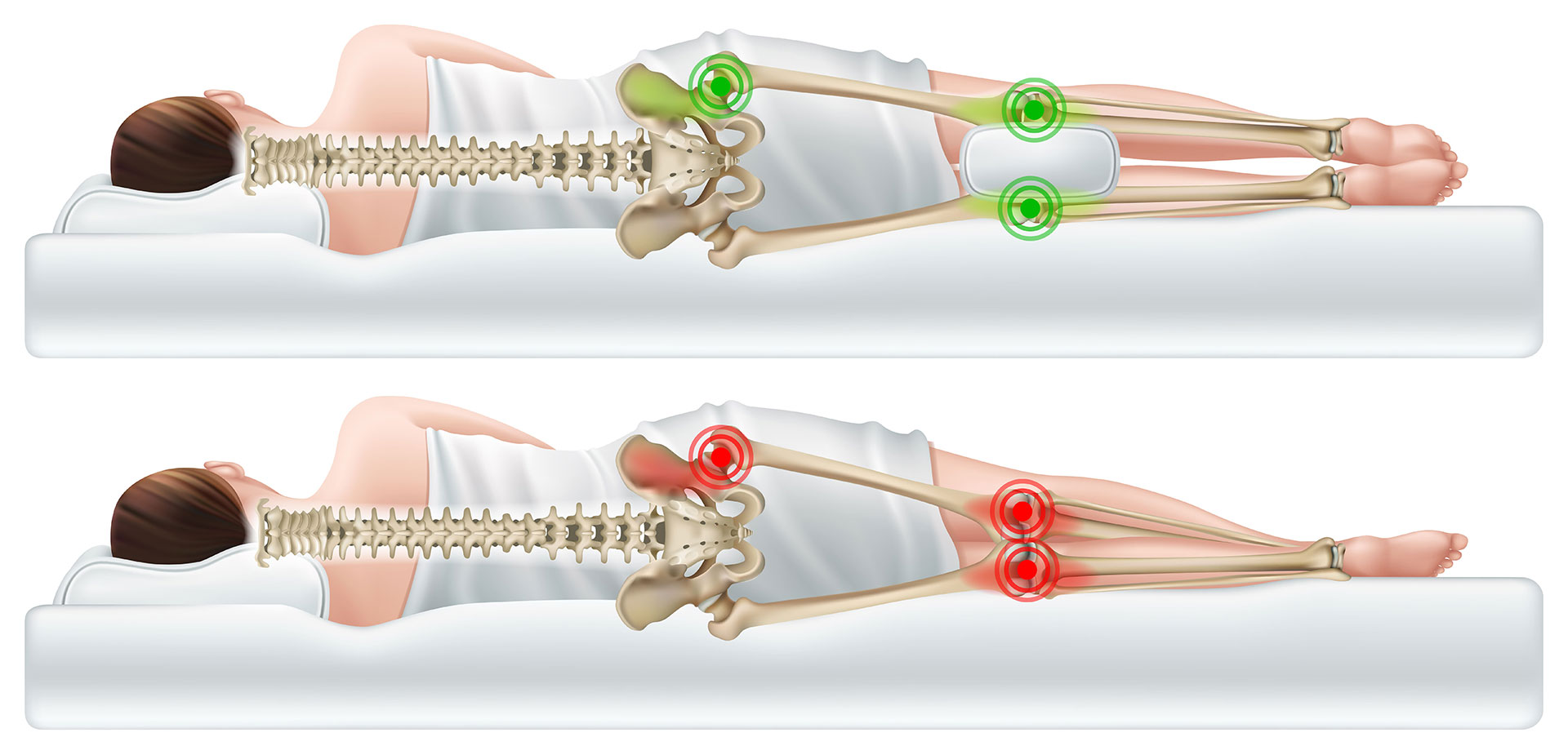
Patients will commonly complain of pain whilst lying on their side in bed combined with pain whilst standing on one leg and whilst climbing stairs (Fearon et al, 2013). It can be diagnosed by your physiotherapist, who will carry out a series of clinical tests to ascertain if you have this condition and to ensure the pain is not coming from other sources such as your lower back or hip joint itself (Fearon et al., 2013)
2. What causes GTPS?
GTPS is more common in female patients aged 40-60 years of age and with those with pre-existing low back pain, osteoarthritis of the knee and knee pain (Williams and Cohen, 2009).
Although GTPS can be associated with a specific injury such a falling onto the hip and/or overuse such as increasing your running too quickly, the exact cause is often unknown.
3. How do we treat GTPS?
In 2001, a study investigating MRI findings of patients with GTPS found that nearly all patients had evidence of gluteus medius tendinopathy associated with bursitis. In comparisons the study found that very few patients had isolated swelling of the bursa (bursitis) (Bird et al., 2001). The primary structure involved in GTPS is therefore likely to be the tendon (tendinopathy) and so exercise should form an integral part of your treatment programme. Shockwave therapy is an excellent adjunct in the treatment of tendon problems.
The first priority when treating GTPS is to get the pain under control. This may include the use of oral medication, modification of activities and targeted prescriptive exercises. This may initially consist of:
- Reducing the aggravating activities
- Avoid standing on one leg for prolonged periods of time
- Modifying sleeping positions – we would advise not sleeping on the painful side and placing a pillow between your knees (see below)
- Targeted hip and core strengthening exercises
- General lower leg strengthening exercises
- Ultrasound guided steroid injections
Strengthening of the hip muscles is vital in the treatment of GTPS and a return to full function. In runners, treating GTPS can vary from strength training of the hip and lower leg muscles to altering running mechanics.
Modifying the load of runners is also crucial, which may include reducing the frequency, duration and intensity of your runs. Your physiotherapist will design a bespoke programme to modify your training load.
4. Is Shockwave Therapy effective for GTPS?
Shockwave has been shown to be very effective in the mid to long term (4-15 months) outcome in reducing pain and increasing the function of those patients suffering with GTPS (Barratt et al, 2017, Carlisi et al., 2019).
Where pain is limiting the ability of the patient to walk and participate in rehabilitation, shockwave therapy has been shown to be effective in reducing the pain in the short and mid-term (Carlisi et al., 2019). This creates a window of opportunity for the patient to commence and undertake rehabilitation guided by the physiotherapist.

5. How many sessions and how often do you need shockwave therapy for GTPS?
At Complete Physio we are guided by the latest-evidence based research for our shockwave protocols. A minimum of 3 shockwave sessions, one week apart is recommended. Some patients will require additional sessions, but this will depend on the patients response to treatment.
6. How long does it take to recovery from GTPS?
Unfortunately, there is no quick fix. Recovering from GTPS can take from 3 to 9 months. The NICE guidelines which guides best practice within the NHS setting highlights that at
12months there is a 72% improvement with exercises that rises to 78% when combined with shockwave therapy (NICE, 2011).
7. Should you have an ultrasound scan before having shockwave therapy?
It is not necessary to have an ultrasound scan before embarking on a course of shockwave therapy. Your physiotherapist will carry out a full assessment of your hip and surrounding structures and will be able to confidentially make a diagnosis of GTPS. They will also assess your lower back and hip joint to ascertain is there if there is any other contributing factors or structures involved.
If your physiotherapist is unsure of the diagnosis they may refer you for an ultrasound scan, with one of our physiotherapists, before commencing shockwave therapy.
If you would like to book an appointment or would like more information before booking please call 020 7482 3875 or email info@complete-physio.co.uk
Other shockwave related articles:
- Patella tendinopathy
- Insertional Achilles tendinopathy
- Mid-portion Achilles tendinopathy
- Injection therapy for greater trochanteric pain syndrome (trochanteric bursitis)
References :
NICE guidelines Treating greater trochanteric pain syndrome using shockwave therapy January 2011
Don’t let pain hold you back, book now!






Leave A Comment