What is patellar tendinopathy?
Patellar tendinopathy is a common overuse injury that typically affects active individuals who play sports that involve a lot of jumping (e.g. volleyball or basketball) leading to the nickname “jumper’s knee”. However, it can also affect runners and players of field sports that involve quick changes of direction such as football and hockey (Reinking, 2018).
The patellar tendon is located on the front of the knee just under the patella (knee cap). It extends from the bottom edge of the patella (knee cap) and connects on to the shin bone at a bony landmark called the tibial tuberosity. Pathology and symptoms usually occurs at its origin on the patella (knee cap) but it can be experienced lower onto the tibia.
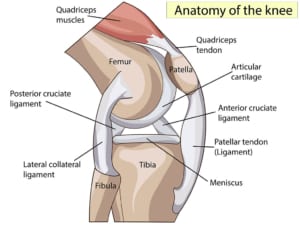
Anatomical diagram of the knee showing bones, tendons, ligaments and muscle.
What causes patellar tendinopathy
There are many other factors that can contribute to developing patellar tendinopathy, some that cannot be changed including genetics and your anatomy, and others that are more modifiable such as training load, muscle strength and flexibility.
Some of the more commonly identified risk factors are below (Reinking, 2018). For some people there may only be one factor at play – a rapid increase in training load for example – whereas for other there may be multiple risk factors:
- A high number of weekly training sessions and/or a rapid increase in training volume or intensity.
- Reduced quadriceps and hamstring flexibility and/or strength.
- Sport specialisation – single sport athletes had a four times greater risk of developing patellar tendinopathy in compared to multisport athletes in one study.
- Patella alta – this is when your knee cap sits higher than normal on your knee. This cannot be modified.
- Movement patterns such as stiff legs when landing. These can be changed through physiotherapy.
- Altered foot and ankle mechanics.
How do we treat patellar tendinopathy?
Most tendon issues resolve with a tailored physiotherapy program but it can take 6-12 weeks particularly if your symptoms have been present for longer than 3 months.
The mainstay of rehabilitation is managing the ‘load’ the tendon is dealing with. ‘Load’ refers to how much force is placed on the tendon. Tendons don’t tend to respond well to complete rest so it is often a case of adjusting your training program whilst improving the capacity of the patella tendon. This is done with a structured loading program involving heavy, slow resistance work that is progressed over time. The programme will focus particularly on your quadriceps strength (the muscle on the front of the knee), but also your gluteal and calf strength.
Other issues that have been identified as potential factors in you developing patellar tendinopathy, such as reduced flexibility, can be addressed alongside the loading program.
If you are not improving with this approach, then the next step maybe a course of shockwave therapy.

A Parkour athlete leaps over a wall
Is shockwave effective?
Yes, shockwave therapy is an effective treatment modality for patella tendinopathy. A review of the literature shows that shockwave is a safe and effective treatment for patellar tendinopathy, particularly in those for whom other non-operative treatments have failed, as well as those who are looking to avoid invasive intervention i.e. surgery (Schmitz et al., 2015, Mani-Babu et al., 2015, Moyer et al., 2018, Korakis et al., 2018).
A study of 66 patients (Furia et al., 2006) found a significant improvement in the reported pain levels of patients receiving shockwave. This amounted to an approximate reduction of almost 50% after 1 month and by 3 months the pain levels had reduced to 25% of their previous levels. Similar results were found in terms of function and by the 12 month follow up mark almost 80% of patients in the shockwave group were happy with their outcome compared to less than 40% in the control group.
Maffulli et al (2018) also found similar improvements following a course of shockwave treatment. All measures of pain, function and satisfaction with treatment were significantly improved at the 1, 3 and 12 month stages.
In a study of 30 knees with patellar tendinopathy, Wang et al (2007) compared shockwave to usual conservative care including nonsteroidal anti-inflammatory drugs, exercise program, physiotherapy, and the use of a knee strap. At follow up, 90% of the shockwave group had satisfactory functional outcome compared to only 50% in the conservative care group. In addition to this greater improvement in function, only 13% of the shockwave group suffered a recurrence of their symptoms compared to 50% of the usual treatment group.
As well as performing admirably when compared to usual care, shockwave therapy also performs well when compared to surgery. Peers et al (2003) found comparable functional outcomes for shockwave treatment and surgery. With shockwave being a non-invasive treatment, it avoids the risks of having a surgical procedure and has consistently been shown to be incredibly safe (Schmitz et al 2015, Moyer et al 2018)
The evidence supports our clinical experience at Complete that shockwave combined with a structured rehabilitation program is the best approach to treating patellar tendinopathy.

A shockwave specialist providing shockwave therapy to a patient with knee pain
How many sessions and how often do you need shockwave therapy for patella tendinopathy?
At Complete we usually recommend at least three sessions at weekly intervals. This is based on the latest research and evidence-based recommendations. Sometimes patients require more than three sessions. This is dependent on your response to the initial course of treatment and whether additional sessions are likely to further help your recovery.
How long does it take to recover from patella tendinopathy?
No two tendon issues are the same but it is certainly not unusual to feel an immediate change in your symptoms following your first shockwave session. Most frequently you will experience a gradual decline in your symptoms over the coming week and months.

Should you have an ultrasound scan before having shockwave therapy?
Not every patient will need an ultrasound scan before commencing a course of shockwave therapy. Your treating physiotherapist will take a thorough history and physical examination to determine the best course of action and whether imaging is required before having shockwave therapy.
An ultrasound scan can be useful to assess the severity of your tendinopathy, exclude a tear, and look for the presence of a bone spur. At Complete an ultrasound scan can be carried out without a GP referral and for no additional fee. Please inform the reception team when booking your appointment that you would like a diagnostic ultrasound scan.
If you would like to book an appointment or would like more information before booking please call 020 7482 3875 or email info@complete-physio.co.uk
Other blogs on Shockwave Therapy written by our specialists
- Calcific Tendinopathy of the shoulder – Shockwave Therapy treatment
- GTPS (hip) – Shockwave Therapy Treatment
- Mid-portion Achilles Tendinopathy – Shockwave Therapy Treatment
- Insertional Achilles Tendinopathy – Shockwave Therapy Treatment
- Our mandatory consent form to be completed prior to receiving Shockwave Therapy from us
References:
Don’t let pain hold you back, book now!







Leave A Comment